Special Enrollment Period for individuals no longer eligible for Medi-Cal
BY WAYNE GUZMAN
It has been more than two years since the public health emergency was declared on March 18, 2020. Since then, new federal laws have been passed to help families, individuals, and businesses during this pandemic, including the Coronavirus Aid, Relief, and Economic Security Act (CARES) and the FFCRA Families First Coronavirus Response Act (FFCRA). These acts included many elements, such as expanded unemployment and disability programs, new employer tax credits and loan programs, extended tax filing dates, and much more.
Still, one area that may not be top of mind when we think of these new laws was the assurance that those who have been on Medi-Cal were not removed from this program during the public health emergency. As a result, the percentage of the existing Medi-Cal population pending possible termination has swelled over the last two years. Well, that is very likely to change in 2022 as it is quite probable that we will move out of the public health emergency, and those no longer eligible for Medi-Cal will be removed from the system and directed to other sources for obtaining their state-required health insurance.
HOW BIG, HOW MANY AND WHEN?
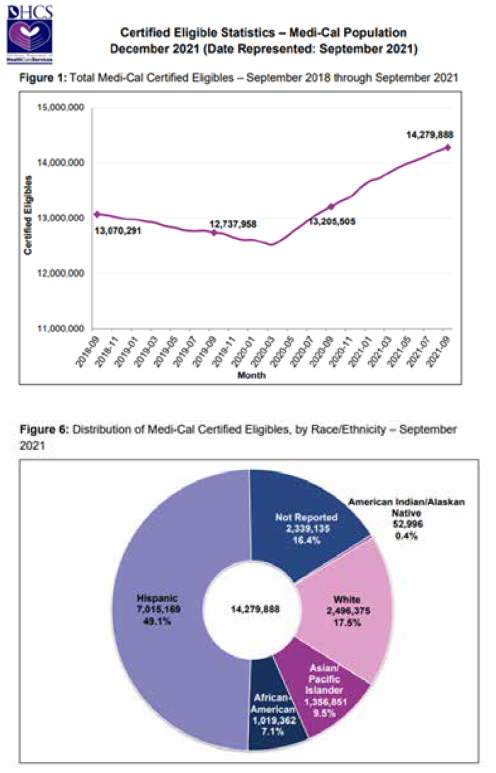
Current estimates indicate that of the more than 14 million individuals currently on the California Medi-Cal program, between 10 and 20% will likely no longer be eligible for Medi-Cal. This will create a Special Enrollment Period (SEP) where they will need assistance in choosing a healthcare plan suitable for them and their families generally within 60 days of losing their coverage. With these events likely to begin between July and September of this year, it is important that agents begin to prepare accordingly.
The good news for agents is that the redetermination will occur over 12 months and not all at once. Covered California will continue to let agents know of prior Covered CA clients who are losing Medi-Cal; moreover, under California SB 260 they will be assigned and the agent simply needs to help the individual affirm.
HOW CAN CERTIFIED AGENTS HELP?
Agents should be mindful and recognize that most of these individuals have been on some sort of managed care plan versus Fee-For-Service. They are accustomed to having rich health and wellness benefits including dental via the Denti-Cal program at little to no cost.
Additionally, agents should take the time to understand the dynamics of the situation and familiarize themselves with the following recommendations:
• Understand the Med-Cal population including mixed households: parents/guardians on-exchangeand children on Medi-Cal; and the dual-eligible Medicare population (Medicare and Medi-Cal eligible beneficiaries)
• Leverage Covered California agent notification that makes agents aware when a former client who was eligible for Medi-Cal in the past is now eligible for a Covered California plan.
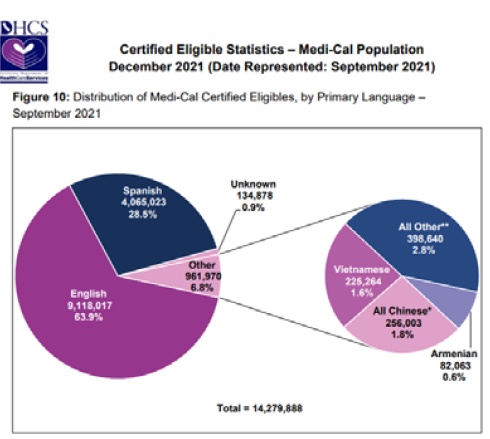
• Offer in-language support and develop cultural competency to understand unique differences among healthcare consumers, including inherent health disparities that exist within the Medi-Cal population.
• Provide educational resources, tools, and develop a contact list and relationship with your local Medi-Cal office.
• Educate yourself by attending workshops and other learning opportunities.
• Remain active and engaged by participating in community-based outreach events focused on supporting this population.
NEXT STEPS?
Since the advent of the ACA exchanges launched on Jan. 1, 2014, California health insurance agents have continually risen to the challenge to help ensure the uninsured by reaching into underserved diverse communities and connecting with community members and leaders often where the agents live and work. These agents have helped many individuals navigate the complex health system and obtain affordable quality health insurance coverage, whether on-exchange, off-exchange, through Medi-Cal, or Medicare. Once again, we can demonstrate our unique value and dedication to helping all Californians by delivering education and personal service during the upcoming 2022 Medi-Cal redetermination.
For more information on how you can help in 2022, please feel free to contact: Wayne.Guzman@blueshieldca.com.

WAYNE GUZMAN, SHRM-SCP, is senior manager, Statewide Outreach for Blue Shield of California. He also serves as LAAHU Diversity, Equity, and Inclusion Committee chair; NAHU Diversity, Equity, and Inclusion Committee past chair and member; and IEAHU past president.
Guzman joined Blue Shield in September 2020, and in his current role oversees a team dedicated to serving the health and wellness needs of our many diverse communities throughout the state.
Since 1989, Guzman has worked in the insurance and financial services industry, successfully helping employers understand and solve some of their most challenging issues especially in the areas of health insurance, employee benefits and compliance.
He is a graduate of California State University, Long Beach with a B.S. in Business Administration-Finance. He also holds industry certifications with the Society for Human Resource Management, AHIP, Covered California, as well as his California Life, Accident and Health, and Property & Casualty insurance licenses.
Guzman grew up and resides in Southern California actively volunteering and serving in many non-profit organizations including the Hemophilia Foundation of Southern California, Cedar House Life Change Center, the Diversity, Equity, and Inclusion Committees for the Los Angeles and National Association of Health Underwriters, and the Society for Human Resource Management. Contact: Wayne.Guzman@blueshieldca.com
