 Private Exchanges–Leveraging Private Exchanges: Brokers Should Advocate Single, Mobile Technology Platforms
Private Exchanges–Leveraging Private Exchanges: Brokers Should Advocate Single, Mobile Technology Platforms
by Robert Oscar, R.Ph. • Mobile apps allow health plans to meet complex challenges in today’s fast-paced world.
Long-Term Care (LTC) Insurance – Reinvigorating the Market by Rethinking the Sale
by Eric M. Williams • Advisors often recognize the importance of LTC insurance in financial planning, but many consumers still resist buying it. Denial can be hard to overcome.
Why You Don’t Need Multiple Illustrations to Sell Long-term Care Insurance
by Cindy Eisenhower • If you don’t do a thorough job of fact-finding before you show an illustration to a client, you run the risk of transferring your own beliefs and preferences into a sale.
Rethinking LTC Sales in an Evolving Market
by Jack B. Schmitz, CLU, ChFC, CASL • These days, new rate-stabilized products in addition to liberal home care features can offer a million dollars worth of coverage for only a few hundred bucks a month.
Medicare Supplements
Medicare Supplements — Know the Guarantees
by Margaret Stedt, C.S.A, LPRT • It’s hard to predict the long-term future for the Medicare supplement plans under ever-changing state and federal regulations. But today’s Medicare supplement plans continue to be an important option for Medicare covered beneficiaries.
Annuities
Leave Volatility and Low Yields In the Past
by W. Andrew Unkefer • How annuities can give your clients the assurance of good planning and lifetime income.
Dental Judgement Day
Get Help with the Tall Order of Deciding on Dental Plans with our Annual Survey!
We’ve asked the top dental providers in California to answer 28 crucial questions to better help you, the agent, understand their benefits, features, and services. Read the second batch of responses and sell accordingly. Part III of the survey will appear in our September issue.
Travel Insurance
Travel Health Insurance: Protect More Than the Itinerary
by Brendan Sharkey • Why you should encourage your clients to ensure their safety and financial protection through the purchase of travel health insurance.
Life Insurance
Understanding the Full Value of Life Insurance
by David Hayward, CLU, ChFC, FLMI • Most consumers don’t object to owning life insurance; they just don’t understand all the benefits it offers.
Individual Health
The New World for IFP Agents with the Exchange & Tax Credits
by Garrett Viggers • Do your individual and family plan (IFP) clients and previously declined applicants, understand their options?
Voluntary Benefits
The Upside of Health Care Reform for Producers: Voluntary Benefits
by Adam Michaels • While producers search for ways to meet client needs, solutions that were once offered without adding budgetary costs have now become an imperative.
Marketing
A New Marketing Plan for a New Market
by Joe Navarro • What we are all about to experience is an advertising/marketing/word of mouth Tsunami like we have never seen before and health insurance will be center stage for months to come.
Private Exchanges–Leveraging Private Exchanges: Brokers Should Advocate Single, Mobile Technology Platforms
by Robert Oscar, R.Ph.
The Affordable Care Act (ACA) challenges brokers to find solutions to complex business issues, rather than simply selling a product. For now, the U.S. government has pushed back the deadline for the employer mandate to 2015, and will not penalize businesses that fail to provide health insurance next year.
Nevertheless, brokers should take advantage of this delay to help clients prepare. Brokers represent an important piece in this puzzle, expertly guiding clients in purchasing the right plan. Therefore, brokers should consider offering private exchange solutions that offer consumers convenient, streamlined information and access. Mobile technology platforms that feature Smartphone apps and online tools help consumers use their health plan benefits more appropriately.
Many consumers are likely to choose high deductible health plans with lower monthly premiums. Pharmacy-specific tools and applications can help customers understand and manage potentially higher prescription drug expenses that come with their new health plan coverage.
A Single Technology Platform
With the private exchange model, employers give employees money to purchase coverage. Employees then pick a coverage level and insurance network based on health needs, employer contributions, provider network participation, and risk tolerance.
The following are some optional features of a private exchange:
• Ancillary Products — voluntary insurance products like dental plans and life insurance as well as property and casualty products, such as auto insurance, and discount cards.
• Shopping Tools — price and quality transparency tools that are critical to a consumer-directed strategy.
• Administrative Services — integration with third-party administrators that provide health savings accounts (HSAs), health reimbursement arrangements (HRAs), and flexible spending accounts (FSAs).
A single technology platform should integrate data from the health plan, pharmacy benefit manager (PBM), and other sources into a single member-centric data set that is accessible from multiple software solutions. For example, the platform could include the following:
• The ability to pull data from one database to another.
• Analytics: Automated and proprietary pharmacy rules and algorithms.
• Embedded security.
• Multi-user access and reporting.
• Configurability by the client.
The platform should also support national health insurance plans, as well as regional providers and payers, pharmacy claim data from every major PBM, daily processing of every plan member, and all major drug compendia.
In an increasingly complicated healthcare environment, health plans must be able to access the data easily in order to design more effective and advanced pharmacy benefits and demonstrate the value of their programs. To enable ever more complex medication regimens and benefit designs, a single platform should automate prior authorization and retrospective utilization management programs.
Anytime, Anywhere
A mobile application suite should offer mobile decision-support tools to members and be configurable. It should do the following:
• Allow members to check their medication history and look-up drug information.
• Provide drug savings calculations.
• Offer plan benefit options.
• Send personalized messages.
• Offer biometric trackers.
• Offer applications that help members prepare for physician office visits.
Health plans should offer a comprehensive mobile technology solution. Mobile technology enables health plans and PBMs to interact with members and providers anywhere they have their mobile phones, whether it’s at the point-of-care, pharmacy, or home – and at any time of the day.
Furthermore, a mobile platform can enable employers to offer more insurance options, simplify the enrollment process, engage health plan members, improve compliance, and help employees get the greatest possible benefit of their healthcare services.
New mobile technology tools with user-friendly enrollment systems allow members to learn about their health coverage, submit reimbursement forms, and find insurance information.
At the moment, health-related apps are used primarily for retrieving information, with some mobile devices providing more one-on-one interaction. For example, a mobile platform can deliver personal drug utilization information to each plan member, including money-saving suggestions.
By providing access to health data, health plans can help members increase prescription drug adherence, reduce emergency care costs, and improve the quality of their healthcare. Apps can also be decision-support tools for healthcare providers and PBMs, allowing them to quickly suggest additional prescription drug purchasing channels, such as mail order and retail discount options.
A member can do the following with mobile Smartphone apps:
• Display the electronic ID card.
• Access a physician directory and get directions to network facilities and physician offices
• View claims.
• Access eligibility and cost-sharing requirements for a given visit.
• See the health-savings account balance.
• View coverage and out-of-pocket totals.
• Look up drug prices at nearby pharmacies and find generic and therapeutic alternatives.
• See allergy and weather information.
• Buy insurance coverage.
• Meet fitness and nutrition challenges and share their accomplishments via social media
Having a mobile strategy can also streamline the management of chronic diseases and reduce the cost burden of unhealthy lifestyles and aging populations.
Lowering Costs
A collaborative technology platform can improve quality and reduce costs with the following:
• A Web-enabled, end-to-end prior authorization management solution.
• Automated intake, routing, criteria verification, letter generation, and approval processes.
• Integrated full Rx history, benefit, and eligibility information.
• A rules-engine that employs all available clinical data and contains standard guidelines.
• Fully configurable codes, letter templates, and reports.
• Compliance with NCPDP-ePA and associated guidelines.
This kind of solution can reduce the administrative burdens of manual prior authorization and improve prior authorization enforcement. It can also document all activities automatically to reduce the approval response time and improve the physician’s understanding of lower-cost therapeutic alternatives.
Personal Touch
It’s important for health plans to interact with members using mail, interactive voice response, and other outbound technologies while automating a high-quality explanation of benefits. Health plans, PBMs, and third-party administrators can use daily member pharmacy claims to generate personalized communications about pharmacy cost-saving and drug-switching opportunities as well as drug interaction alerts.
A Single Point of Access
There are key advantages to placing pharmacy and therapeutic decisions into a single Internet accessible database:
• It reduces administrative burdens.
• It reduces the time it takes to create formulary benefit designs and reduces the potential financial impact to plan sponsor.
• It reduces costs and decrease formulary errors during claims processing.
• It increases federal and state reporting compliance.
• It facilitates formulary reporting to plan sponsors.
It should do the following:
• Transmit formularies automatically to e-prescription hubs and vendors and synchronize updated formulary information for provider systems.
• Employ a graphic user interface design that makes it easy for clinicians to query, update, extract, and communicate the formulary data.
• Support multiple drug identification compendia (summaries of drug information, which compiled by experts who have reviewed clinical data on drugs.)
Conclusion
Mobile apps allow health plans to meet complex challenges in today’s fast-paced world. An optimized mobile-platform technology strategy makes it easier for health plans to meet members where they want to meet– primarily at the employee and member’s convenience.
It is possible to meet health reform goals to streamline the flow of information, close gaps in care, and shorten medical response times. But brokers must play an integral role in guiding change. Privately run exchanges with participating insurers will need to provide instant access to information. A single-source technology platform that offers online tools can improve member behaviors and lower rates by improving health and productivity of the workforce.
–––––––––
Robert Oscar, R.Ph., has more than 25 years of experience in healthcare. Throughout much of his career, Oscar has developed and implemented successful programs to effectively manage pharmacy benefit risk including pioneering work in the Medicare HMO market. Before founding RxEOB more than a decade ago, Oscar worked in the medical information systems industry, designing, developing and implementing several different claims analysis tools. Licensed in Virginia and certified in pharmacy-based immunization, Oscar is a graduate of Ohio Northern University. Contact info: info@rxeob.com.
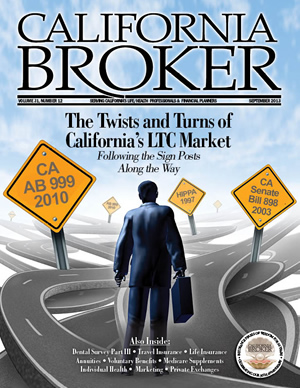
The Twists and Turns of California’s LTC Market
In this issue, our authors take on long-term care challenges from multiple angles. Advisors are urged to look beyond traditional coverage to design policies for underserved consumers — not only those who can’t afford traditional LTC insurance, but also those who prefer to self-insure much of their potential LTC costs. Our authors explain how to engage clients in the policy design process and push through the consumer’s denial in order to sell coverage that can truly protect house and home.
LTC Insurance- Reinvigorating the Market by Rethinking the Sale
by Eric M. Williams
Advisors often recognize the importance of LTC insurance in financial planning, but many consumers still resist buying it. We’ve all heard the reasons. Some don’t think they will ever need long-term care. Others expect to rely on family members or government programs. Denial like this can be hard to overcome.
There are also the savvy consumers who recognize the value of LTC insurance. So why aren’t they buying? The reason is that they just can’t afford it. That’s why it’s time for the industry to rethink LTC insurance. Less expensive alternatives to traditional coverage will create opportunities by meeting the needs of a different set of consumers. And learning how to identify the best prospects will open the door to more sales for agents.
The Affordability Factor
There may always be a market for traditional LTC insurance, with 5% compound inflation and all the accompanying bells and whistles, but it comes at a cost. Seventy-four percent of consumers who said they would not consider purchasing LTC insurance, cited cost as the primary reason, according to a 2012 John Hancock study conducted by Forbes Consulting Group. The same study showed that sixty-four percent of consumers would choose basic LTC coverage at an intermediate cost over traditional LTC coverage at a higher cost. Even small premium decreases led to noticeably stronger intent to purchase among all consumers.
Rethinking the Sale for a New Audience
With these results in mind, it may be time to broaden your audience and rethink your sale. The traditional LTC insurance sale has focused on the more affluent retired person or on people who are on the verge of retirement. But these consumers are not the only ones who need this valuable coverage, particularly in California where care can be costly. It’s time to start marketing less expensive coverage to a new set of consumers who face the same financial risks as traditional clientele.
One group to target is made up of younger LTC insurance consumers — people in their 50s who may be in the workforce for many more years. These prospects may have competing financial priorities, such as a mortgage or a child’s college tuition, but this shouldn’t preclude them from affording LTC insurance if they are willing to consider alternatives to a traditional plan design. You can start the conversation by pointing out that, at this age, the need for long-term care could last a long time, and being prepared may be the most prudent approach to address the potential risk.
Starting with the inflation feature is a good way to keep the premiums within reach of younger consumers, especially since it’s one of the primary drivers of policy cost. For a more affordable price point, advisors can consider Consumer Price Indexed inflation protection. It provides -annual compounded benefit growth that is tied to changes in the Consumer Price Index for All Urban Consumers — one of the most trusted economic indicators. Carriers that offer this option can hedge much of their investment risk, which allows them to offer a much more affordable price.
Or, you can also consider using other inflation alternatives like 5% simple or 3% compound. There is also the option to write a policy with no inflation protection coupled with a larger daily benefit at the time of purchase. The point is that you need to think creatively to balance protection with affordability.
Also underserved are people who can self-insure a portion of their long-term care expenses. They usually have higher net-worth than do younger consumers. Even if they think they can fund an LTC event out-of-pocket and may view LTC premiums as a waste of money, you can explain how LTC insurance can limit their financial liability if care becomes necessary. You can recommend a policy that doesn’t necessarily cover the full cost of care where your prospect lives with the understanding that will assume liability for any expenses in excess of the insurance benefits. This can be accomplished by having lower daily/monthly benefit amounts, a longer elimination period, or by omitting optional features.
How to Identify Potential Buyers
These two consumer groups hold promise for new sales. But to capitalize on an expanded marketplace, you need to identify who is most likely to buy. People who are characterized as planners make the best prospects, particularly married couples. A previous study by Forbes Consulting Group for John Hancock identified planners. Some motivating factors for this group include a desire to maintain their independence and protect their families from the financial and caregiving burdens of long-term care. They feel responsible for planning ahead for their own LTC needs and they want their potential care to be in the most comfortable setting possible.
Having a simple conversation can be an effective way to identify a planner. People are more likely to consider LTC insurance if they own other insurance products, like life and disability insurance. Planners usually contribute the maximum allowable amount to their 401k plans for retirement and contribute the maximum to 529 plans for their children’s education. While they accept the notion of aging gracefully, they are more likely to engage in a healthy lifestyle with a sensible diet and regular exercise. Most important may be how they respond to a simple question, “Who do you think is responsible for your potential LTC needs?” If they are willing to assume this responsibility, they are likely to be receptive to working with you in designing the LTC policy that meets their needs and satisfies their budgets.
The Future of LTC Insurance
Long-term care continues to be one of the most significant uninsured financial risks. The future of LTC insurance holds enormous potential because it remains one of the most cost effective ways to protect assets and income from the high cost of care. Advisors will be doing their clients and their practices a great service by looking beyond traditional coverage to design policies that are right for underserved groups.
––––––––
Eric Williams is a regional vice president for John Hancock LTC. He is an 18-year veteran of the long-term care insurance industry and has experienced success as a producer, sales trainer, brokerage manager, and home office sales executive. He can be reached at ewilliams@jhancock.com.
Why You Don’t Need Multiple Illustrations to Sell Long-Term Care Insurance
by Cindy Eisenhower
One thing has never ceased to amaze me throughout my 18 years in the long-term care industry working as an agent, wholesaler, consultant and trainer: Even in this day and age, insurance brokers still request multiple illustrations before discussing the need for long-term care planning with their clients. This is one significant reason why the market penetration remains so low. You can’t recommend a relevant policy to a buyer without first discussing the buyer’s wants and needs.
The average cost of care in your area may be X, but there’s no reason to presume your client wants to cover 100% of the risk. Some clients won’t want the average and others will be fine with less than the average. Only by thoroughly outlining the client’s specific problem can you arrive at a reasonable solution. And the definition of “reasonable” is never exactly the same for any two buyers.
If you don’t do a thorough job of fact-finding before you show an illustration to a client, you run the risk of transferring your own beliefs and preferences into a sale. When doing this, we often transfer our own limitations as well.
Years ago, I worked with a couple in the San Francisco Bay Area. This couple was adamant about their preferences. They wanted the most daily benefit available, unlimited benefit duration (which was available at the time), the least number of days for the elimination period, the best inflation coverage, and to have a 10-pay policy. Since the per-year premium for each of them was $30,000, the total annual premium was $60,000. In my opinion, it was way too much coverage, but that is what they wanted.
And that is what they purchased.
We salespeople sometimes overlook the financial diversity of those among us. Some drive Bentleys; others don’t. Regardless, people purchase what they want and what they can afford. In the example above, neither buyer wanted their children burdened in any way when it came to their potential need for long-term care. In other cases, I have seen couples who felt they could afford to self-fund a portion of their risk, which led to them purchasing a minimal policy. I have also encountered a single person who had an investment fund set aside. He felt that he could use the fund dollars to augment his policy in regard to the inflation risk. So he passed on buying inflation protection.
There is no universal fact-finding standard for our product. Other financial products have them, but ours does not. Many of us can remember when asset allocation was mandated for all investment brokers. It was there to test our clients’ investment tolerance and determine the appropriate investment portfolio for each one.
In light of the general lack of a universal standard, our firm went ahead and developed one. Before we did so, our brokers felt vulnerable. They simply had no dependable vehicle for asking questions and documenting answers. Many brokers at many firms continue to feel this way. Time and time again, I hear these questions, “How can I document what the client is purchasing to avoid any unpleasantness in the future?” and “How will I know that the long-term care policy I have designed for and sold to my client is appropriate?” The key is to ask every client the correct questions.
So what makes for a good fact-finder when it comes to long-term care planning? For starters, after making clients aware of the need to plan, ask where they plan to live later in life. Then remind them (subtly) who is going to pay the bill if they don’t transfer the risk. A good first question might be, “At the rate of X (the average cost of care where you plan to live) how many years could you afford to pay for your own care?”
In essence, you have just asked, “How much money do you have?” But you have asked in a respectful way — a way that shows that you’re mindful of when the money might run out.
Next question, “Where do you keep your funds? nutual funds? CDs? money market accounts? Etc.?”
Upon hearing the answer, you know where the money is and — more importantly — where the 1099s come from. You have effectively uncovered additional possibilities for sales. You may now be able to re-position an asset to create the premium, which is positive because, in my experience, when you find the premium you’re that much closer to clinching the sale.
“What rate of return do you expect on your investments?” Here you’re seeking a general idea of how much they’re earning. Upon finding out, ask if they live on any of their investment earnings. In other words, overall, you’re asking, “What is your income and where does it come from?”
Your job is to protect both the principal they have accumulated and the family they love. The interest they earn on their investments may be another means of funding the premium.
“How important is it for you to leave a legacy?” This question produces new information (as do all the others), which helps to determine the policy design.
In truth, only four components of a traditional long-term care policy need to be addressed. All the additional riders just function to answer objections. The four components are as follows:
1. A daily/monthly benefit amount
2. Benefit duration
3. Elimination period
4. Inflation protection
And that’s it! You may be in love with the restoration of benefits rider, but your client may not see the need to add it on and pay for it. So start with the four components above, and reserve the riders for dealing with objections.
Getting back to the earlier question, “If the cost of care in the area you plan to reside in is X, how much of that would you feel comfortable paying out of your own resources?” If the answer is, “None of it,” you still have a baseline in which to work.
Keeping X as your baseline, find out if they are comfortable paying 50%. If they are, propose that they pay 50% of X. From a psychological perspective, you are now guiding the discussion in a way that helps the buyers design their own policies.
To determine benefit duration, discuss longevity and family history. A client with nine different relatives who lived for 20 years with Alzheimer’s disease may want longer benefit duration than one whose family members generally passed away at a younger age.
While you should use the averages, you should also discuss family history and longevity. This puts them in mind of family members who needed exactly this type of care (and even the ones who didn’t yet still of course, grew old).
Meanwhile, discussing the elimination period is just like discussing a deductible on any other type of insurance: “If the worst case scenario happened, how many days of care could you afford to pay for before the policy paid a benefit?”
This is where you could use a rider for a 0-day home care elimination period. Or you can remind them of that rainy day money account they mentioned, which they could use for paying the elimination days.
Inflation protection makes for an important discussion, as well. Again, it should revolve around how old they are, what their resources are, and whether they want to use their resources to cover this risk.
At this point. you have enough information to run an illustration because you have included your client in the process of designing a policy that is actually relevant to them.
Bear in mind that software programs are available to aid you in showing them a computerized illustration, right there on the spot. If the premium is uncomfortable, make adjustments. If objections start surfacing, explain the riders that can be added. For example, you may hear, “What if I die and never use the insurance?” I’d answer, “That would be the policy I hope to pay for, but if it makes you uncomfortable, we can add the return-of-premium rider.”
Or point out that certain companies include a return of premium up to a certain age. “What if I am in an accident and need care and then recover? Will I use up my insurance too soon?” When replying to this, discuss the restoration of benefits rider and explain the cost.
Invariably, the objection you will hear the most is, “That is just too expensive.” So ask your client, “Expensive in relation to what?” In many instances, you may need to point out alternative options, “Would you like to pay $5,000 a year, or $5,000 a month?”
In most cases, if your client pays into a long-term care traditional policy for 30 years, it will take about 90 days to get all the premiums paid back in benefits later on, which is not a bad return if you consider the other option.
In addition, premium increases should be discussed. If your client would not be able to keep the policy in force if the premium were raised in the future, they may not be a suitable match for this type of plan. Perhaps a hybrid life/long-term care policy or an annuity/long-term care policy would be more in line with their needs and resources.
But until you have engaged them in the process, you will not really know. Having worked with some of the best life insurance brokers, financial planners, and investment brokers around, I can state, with confidence, that the most successful ones give their clients the best solution, not five or six different ones.
In the end, you don’t truly need illustrations to sell financial products; what you need more is conviction. When you engage your client in the policy design process, you open the door to a solution that is relevant to them. Yes, this takes time and energy, but the outcome will be stronger for it. And your clients – many of whom will become your friends – will always end up being better off.
–––––––––
Cindy Eisenhower is director of LTC Sales for Leisure Werden and Terry Agency.
Rethinking Long-Term Care Sales in an Evolving Market
by Jack B. Schmitz, CLU, ChFC, CASL
The world of long-term care insurance has evolved a great deal in the past 18 months, but the most monumental change occurred on January 1, 1997 when the Health Insurance Portability and Accountability Act (HIPAA) went into effect.
HIPAA established a new class of federally tax-qualified LTCI policies, set requirements that must be met for a policy to be tax-qualified, and granted favorable tax treatment to the policies that meet those requirements.
HIPAA establishes six standard activities of daily living (ADLs): bathing, dressing, toileting, transferring, continence, and eating. Tax-qualified policies must include at least five of these six and must use the HIPAA definitions. Also, they must define a physical impairment as the inability to perform at least two of the standard ADLs without substantial assistance from another person. This made it much easier for consumers to understand how long term care (LTC) insurance policies pay benefits.
Previously, S.B. 1943 passed in 1993, which stated that comprehensive LTC policies must include specific home and community based language. The bill also required that all LTC must be guaranteed renewable.
It may be hard to believe that LTC insurance didn’t have to be guaranteed renewable before 1993, but this oversight correlates perfectly with some of the unbelievable LTC products being sold before 1993. The buyers may have thought of it as insurance for LTC, but it barely even paid for nursing home stays. Some of the plans essentially supplemented Medicare and required a three-day hospital stay. Alzheimer’s Disease and other severe cognitive impairments, which account for the majority of LTCI claims, generally do not require a three-day hospital stay, so how often do you suppose these policies paid?
One of the first carriers in the business dared to add home care to its policy. However, it paid for care in the home after you returned home from the skilled nursing facility. Your home care benefit period was only equal to the length of your stay in the skilled nursing care facility. Consequently, more insurance companies began to love the product – a product that people need, but no one wants to use! Everyone avoids the nursing home, and that’s where these older policies paid the most. The insurers could always raise the rates later if they wanted more profit.
To top it off, there were no prohibitions on closing one product pool and starting another. They could offer seemingly liberal benefits and eligibility, but include fine print that the help must be hands on, the elimination period must be met within a short period of time, or the nursing home must have a lab or 16 beds or an RN on staff, etc. The inability to easily determine eligibility for benefits generated enough consumer concerns and complaints to catch the attention of legislators.
In 1997, HIPAA standardized eligibility by requiring that all comprehensive LTC policies use the same list of ADLs and it eliminated disparity in how eligibility is determined. One policy may have required “hands on” assistance while another would require as little as “stand by” assistance to perform ADLs. HIPAA required that the more liberal “stand by” wording be used in all Tax Qualified LTC insurance.
Ultimately, HIPAA did not scare away the carriers. In fact, more carriers entered the LTC business. Until around 2004, the top three carriers had never raised rates on existing business. However, that streak ended shortly after California passed S.B 898.
Rate Stability Legislation
In 2003, Senate Bill 898 made it more difficult for carriers to raise rates. Something more than moderately adverse would need to occur in the economy to warrant a possible rate increase, and even then, the process would involve other restrictions thereby making it more complicated to implement any future rate increase.
However, the law only applied to new business. This is when the majority of the LTC insurance carriers decided that it was a good idea to raise rates on older blocks of business. Carriers that had never raised rates on existing LTCI clients decided to file moderate rate increases on older blocks of business. They increased new business rates 30% to 50% as well, since it would be more difficult to approve rate increases on business written after the new rate stability legislation was implemented. At this point, several carriers left the LTC business.
In 2010, A.B. 999 passed in California with a surprising lack of resistance from LTC carriers. Essentially, A.B. 999 added even more contingencies to get rate increase approval. By coincidence, this legislation was initially written around the same time several top LTC carriers left the market. Others left until their new products could be approved, and yet others introduced another iteration of products with higher rates with some still waiting approval.
Obstacles like interest rates, low lapse rates, claims, and legislative regulation have caused many carriers to leave the LTC market. Now what?
California operates with LTC products that are always one or two generations behind most of the country. Once a company decides that it wants new features and/or a higher premium, it files a new product with the California Dept. of Insurance, and begins a process that sometimes takes years before culminating in an approval. This leaves us with an off-balance market as one carrier receives approval and another doesn’t. In California, the Dept. of Insurance rewards innovation with more hoops to jump through and longer waits. This steers the market in favor of the carrier with the oldest product. And when that carrier introduces a new product, we have a fire sale: increased sales of the older, cheaper product.
Not being able to introduce new products and rates in a reasonable period of time has caused several carriers to leave California and some to leave LTCI altogether. While gender distinct rates and new innovations are being introduced in other states, it seems like we may never see them in California.
Intrinsic Value
Be that as it may, over the past 30 years, LTC insurance has evolved from a primarily nursing home insurance product targeted to those over age 65, to a comprehensive home care product targeted to those aged 50 to 60. LTC insurance keeps you out of the nursing home. It works. Some people may complain about their mother’s old policy not paying, or the article they read about giant rate increases, or companies leaving the market place, but new products possess stronger consumer-friendly safeguards: standardized eligibility criteria using activities of daily living, rate increase limitations, rate stability, non-forfeiture provisions, and some even provide asset protection through state partnership programs.
These days, new rate-stabilized products in addition to liberal home care features can offer a million dollars worth of coverage for only a few hundred bucks a month. This valuable purchase will protect their retirement income and provide peace of mind. Ultimately, LTCI will make life easier for the clients and their loved ones, especially when the devastation of a chronic illness or severe cognitive impairment occurs.
Challenges In the Selling Process
Now that we have arrived to a place with higher rates for this product than we have previously seen, we have had to take another look at what we are offering, and come up with new solutions to wage against the threat of taking retirement income to pay for the exorbitant cost of long term care services. After multiple rate reviews and agent surveys, these are our observations:
People are more worried about rate increases than non-increasing benefits.
Carriers do not like 5% compound inflation, which is now priced as much as three times the price of CPI inflation and two times the price of simple inflation. In a high-inflation economy, compound CPI Inflation may increase benefits higher than 5%.
Having the option to increase benefits without evidence is not always free.
If your spouse/partner isn’t approved you may not get a discount.
Shared Care Isn’t A Panacea With Short Benefit Periods
People over 60 may buy a higher daily benefit with no inflation protection.
CA Partnership plan sales may be sparse until they allow other inflation options.
A starter plan doesn’t have to have inflation protection.
Something Is Better Than Nothing
The bottom line is that advisors need to rethink and resurrect sales using CPI compound, 3% compound, 5% simple, or no inflation designed solutions when appropriate and when in the client’s best interest, and when the alternative is to do nothing. The cost of long-term care services is so high. At the same time an AARP report reveals that, if you live past 65, you will have a 68% lifetime probability of becoming disabled in at least two ADLs or being cognitively impaired. It begs the question: How do you plan to address the issue of long-term care and living a long life?
–––––––––
Jack B. Schmitz, CLU, ChFC, CASL is president – DI & LTC Insurance Services, a brokerage general agency in San Rafael Calif. that provides income protection products and services to California brokers. For more information, visit www.di-ltc.com or call 800-924-2294.
Medicare Supplements – Know The Guarantees
by Margaret Stedt, C.S.A, LPRT
Are you ready to ride the wave? Every day over 10,000 Baby Boomers turn 65. And they’re looking to insurance professionals to help them to understand their options and how Medicare works. Many of our seniors continue to work past their 65th birthday, and are confused about their options, especially as employer plan rates increase and retiree plans terminate.
As a health insurance sales professional, you can help clients and prospects explore these options and find the plans to fit their needs.
Seniors have many coverage options, such as Original Medicare only, Medicare Advantage plans (HMO) employer plans for people continuing to work, and retiree plans. Medicare supplement plans (also called “Medigap”) play an important role. Nearly one in four Medicare beneficiaries has a Medigap policy. The most popular plans, F and C, have the lowest cost sharing.
Medicare supplement plans, which are sold by private insurance companies, are designed to fill in the gaps in Original Medicare (Part A and B) of Medicare. These gaps include the deductibles, coinsurance, and copayments. Ten Medicare supplement plans are offered: A, B, C, D, F (including the high deductible), G, K, L, M and N.
The plans are exactly the same from company to company. However, these aspects vary from plan to plan:
• The rates.
• The rating methodology based on community, issue or attained, and smoking or non-smoking.
• When they change their rates, some underwriting guidelines and plans offered vary from company to company.
Plans H, I, and J are no longer offered for enrollment, although many seniors are still covered under these plans.
There are a multitude of advantages for agents to sell Medicare supplement plans in the senior market:
• There is no annual enrollment period.
• You don’t need a scope of appointment before meeting with the senior.
• The covered individual can access any provider who accepts Medicare within all 50 states and U.S. territories.
• No referrals are required to see specialists and the plans are guaranteed renewable.
• Medigap plans help make health care costs more predictable and stable for the covered person.
• Many companies offer commission renewals for many years and some for the life of the contract.
• Most importantly, many seniors will qualify for coverage under the Medicare supplement guarantee issue situations.
The key to selling Medicare supplements is to understand guarantee issue guidelines. Agents who are confused by the guidelines lose opportunities to help their clients and grow their practice. In addition, some agents only focus on the aging in 65 year olds and miss assisting the older seniors or people under 65 who have qualifying events/changes.
The guarantee issue situations are under federal and state regulations. Many guarantee issue situations are the same from state to state. But the plans that the companies offer and the offer periods for guaranteed acceptance vary from state-to-state. Also varying from state-to-state are the availability of the plans and restrictions for people under 65 who have end-stage renal disease. There is no federal requirement for states to offer Medigap plans to the under 65 Medicare covered persons. In this article we will focus on California.
What is guarantee issue? It means that the applicant must be accepted for coverage regardless of their current health or health history.
Companies that offer Medicare supplement plans in California must offer plans A, C, and F to people 65 and older. They can offer any of the other seven plans. As you review the various companies, look at their underwriting guidelines and guaranteed issue situations as well as what documentation they require with applications.
In order to be eligible for coverage under a Medicare supplement plan, the applicant must be enrolled in Medicare plans A and B (Original Medicare). Also, they must continue to be enrolled while under the Medicare supplement plan.
To determine your client’s eligibility for guarantee issue coverage, you need to see which guarantee issue situations apply and what is required for your clients to enroll. Here are some key questions to ask:
• When did your client begin their Part B coverage?
• If your client has a Medicare supplement plan, when is their birthday?
• When did your client lose coverage (employer, retiree plan, PACE, Medi-Cal, Medicare Advantage, military coverage, or base closures)?
• Were there any changes in -coverage costs with your client’s Medicare Advantage plan?
• Did their share of -Medi-Cal costs change?
• Were there other changes, such as loss of a spouse, etc.?
Applicants Who Are New to Medicare
An applicant who is 65 or older and is newly enrolled in Medicare Part B has six months from the enrollment date to apply for a Medicare supplement plan. They can apply on a guarantee issue basis to any of the plans offered by the insurance company.
The required proof is their Medicare number and effective dates for Part A and B. These applicants can typically choose from all of the Medicare plans that the insurance company offers. Many companies accept applications up to three months before the Part B effective date as long as they have their Part A and B coverage.
Applicants who are under 65 can enroll within six months of receiving their Part B coverage. They can also enroll within six months if they have been notified of eligibility retroactively. They are not eligible if they have end-stage renal disease. (Important Note: the under 65 will have a new guaranteed issue period open up when they turn 65.). Applicants who are under 65 may have fewer plans from which to choose. Also, monthly costs are considerably higher than they are for people aging in at 65.
The Birthday Rule
California is one of the few states that allow a person who is covered under a Medicare supplement to change to an equal or lesser plan every year on their birthday or 30 days afterwards. That means that they can switch from one company’s plan F to another company’s plan F or from a plan F to a plan N, for example. However, in order to change to a higher plan, they would have to answer health-underwriting questions (for example, when switching from an N plan to an F plan). F is the top plan in the hierarchy of plans currently offered.
Remember to check each company’s underwriting rules. Some allow you to submit the application 30 days before the birth date or up to 30 days afterwards. Others require you to write the application from the birth date or within the 30 days after. With one particular company, all plans are available for covered persons to change from month to month.
Also remember that this only applies to Medicare supplement policyholders, not to anyone enrolled in a Medicare Advantage plan. Many agents are confused about the birthday rule. Always submit a signed replacement form and proof of prior coverage with the application.
Loss of Coverage
These guarantee issue situations address the loss of coverage in these situations:
• You are in a Medicare Advantage Plan, and your plan is leaving Medicare or stops giving care in your area, or you move out of the plan’s service area.
• You have Original Medicare and an employer group health plan (including retiree or COBRA coverage) or union coverage that pays after Medicare pays and that plan is ending.
• You have Original Medicare and a Medicare SELECT policy. You move out of the Medicare SELECT policy’s service area. You can keep your Medigap policy, or you may want to switch to another Medigap policy.
• (Trial Right) You joined a Medicare Advantage Plan or Programs of All-inclusive Care for the Elderly (PACE) when you were first eligible for Medicare Part A at 65, and within the first year of joining, you decide you want to switch to Original Medicare.
• (Trial Right) You dropped a Medigap policy to join a Medicare Advantage Plan (or to switch to a Medicare SELECT policy) for the first time; you have been in the plan less than a year, and you want to switch back.
• Your Medigap insurance company goes bankrupt and you lose your coverage, or your Medigap policy coverage otherwise ends through no fault of your own.
• You leave a Medicare Advantage Plan or drop a Medigap policy because the company hasn’t followed the rules, or it misled you.
The opportunity to enroll varies by situation, as does the period to apply for coverage under guarantee issue. The after are the most common:
• Loss of Employee/Leaving Retiree plan coverage – The applicant can apply up to two months before or up to six months after the date termination of coverage. However, an applicant being new to Part B overrules the loss of coverage situation. For an applicant who is not new to Part B, be sure to include a copy of the termination notice or certificate of prior coverage with the application. This situation can also apply to loss of eligibility for converge under the employer or retiree plan due to death of spouse or divorce.
• Loss of Medicare Advantage Plan – Medicare Advantage plans can exit the market during the upcoming annual enrollment period or rarely during the year. Plan members can apply within 123 days of losing coverage. Be sure to include a copy of the termination notice or Certificate of Prior Coverage with the application.
• Loss of Medi-Cal or Increase in Share of the Cost of Coverage – The applicant has up to six months to apply for coverage after the loss of coverage. Along with the application, submit a copy of the notice of termination from the Medi-Cal program or the notice of the increased cost share due to a change in income/assets.
Medicare Supplement/Medicare Advantage Plan Switches
The most misunderstood guarantee-issue situations involve knowing when a Medicare Advantage plan member is eligible for a Medicare supplement plan. The key is knowing when the member first enrolled in the Medicare Advantage plan, whether they were in a Medicare supplement plan before, or whether the Medicare Advantage plan changed the costs of the benefits (for example, copays or coinsurance amounts for any Medicare benefits.) Let’s take them step by step:
First Time Enrolled in Medicare Advantage
Suppose a member first enrolled in a Medicare Advantage at 65 plan and then voluntarily disenrolled from the plan or program within 12 months of the effective date of their enrollment. They can apply 60 days before or up to 63 days after the termination of coverage. A copy of termination or certificate of prior coverage must be submitted with the application.
First Enrolled in Medicare Supplement Then Went to Medicare Advantage Plan
Let’s take the case of a member who leaves a Medicare supplement plan to enroll in a Medicare Advantage plan and then leaves the Medicare Advantage plan within 12 months of their enrollment. They can reapply for the Medicare supplement plan under their prior insurer if it’s still offered. They must include proof of coverage for the Medicare supplement insurer and the Medicare Advantage carrier with the application 60 days before or 63 days after the termination date.
Medicare Advantage Plan Changes
When is a member eligible for coverage under the Medicare Advantage carrier’s Medicare supplement plans? They are eligible if their cost (copayments, coinsurance or premiums) are increased, if any benefits are reduced, or the contract of the provider providing care to a member is discontinued) A member can apply 60 days before or up to 63 days after the termination of coverage. They must submit a copy of termination or certificate of prior coverage notices along with the application.
The second situation applies when costs increase or benefits decrease 15% or more. Suppose that no Medicare supplement plan is available through the Medicare Advantage carrier or its affiliated companies. In that case, a member can apply with any Medicare supplement insurer for coverage under their offered plans. A member can apply 60 days before or up to 63 days after the termination of coverage. A copy of termination or Certificate of Prior Coverage must be submitted with the application.
It is important for you evaluate changes to the Medicare Advantage plan benefits and costs for your clients and prospects, especially during the annual open enrollment period.
Some will need to switch to a Medicare supplement plan because they now have health issues that require multiple providers who are outside of their plan’s network or require great flexibility in treatment referrals. Or, they may find that premiums are too high, out-of-pocket expenses are too high (copays/coinsurance/deductibles), or the maximum out of pocket expense limit is too high. Also, their plan may be leaving the market or their provider group or physician may no be longer affiliated with the Medicare Advantage plan.
Since there are additional guarantee issue situations, you need to do a careful review of the Medicare supplement guarantee situation listings for each company. Most are included in the application kits. For additional information, refer to the Medicare booklet, “Choosing a Medigap Policy.” Remember that this booklet must be provided at the time of application to a Medicare supplement.
There are many tools to help you understand the guarantee issue situations including the www.medicare.gov website, each Medicare supplement company’s websites, sales materials, agent support personnel or your own GA or field marketing organization.
It’s hard to predict the long-term future for the Medicare supplement plans under ever-changing state and federal regulations. But today’s Medicare supplement plans continue to be an important option for Medicare covered beneficiaries. Many seniors don’t understand what Medicare supplement plans cover and when they can change their plans. With your increased knowledge of the guarantee issue guidelines, you will be better prepared to help your clients and prospects know their options and get the coverage that best fits their needs.
–––––––––
Margaret “Maggie” Stedt, C.S.A, LPRT is president of The Hartley Group Inc. and mans Stedt Insurance Services. The firm specializes in consulting services, training, and sales of individual life, health, and group insurance products. She specializes in the senior market. She is a member of the Leading Producer Round Table with NAHU and an Independent Contractor/Licensed Agent and Consultant. AGA is the field marketing office that she has been affiliated with since 2006. Previously, she was with Equitable Life, Mutual of Omaha, Pacific Mutual (now Pacific Life), Transamerica, PacifiCare Life, and Secure Horizons.
Stedt is vice president of Membership for Orange County Health Underwriters, co-chairs a Medicare Builders Agent Group and is also a Distinguished Toastmaster and Certified Lay Speaker.
Annuities–Leave Volatility and Low Yields In the Past
by W. Andrew Unkefer
More than $2.59 trillion is sitting in low-yielding money market funds earning less than 0.50%, according to the Investment Company Institute 2013 Factbook. And the FDIC says that more than $10.8 trillion is on deposit in banks earning yields near or below 1%. In addition, over 92 million Americans have invested more than $11 trillion riding the mutual fund roller coaster. It’s a great time to evaluate options that may be more suitable for your client.
Is it better to play it safe or reach for some growth? Since there are more than $11 trillion in assets in mutual funds, let’s begin with a look at the stock market. Our study will take a look at the S&P 500 Index (excluding dividends) over the 13-year and five-month period ending in May of 2013. How have people fared? See Chart 1 below.
The S&P 500 Index from January 1, 2000 to August 5, 2013
It’s the tale of the tape. The S&P 500 Index is up during this period. In fact, anyone who used a buy and hold strategy during this time would have had a compound growth rate of 1.48%. If your client is sitting on assets, they may not be concerned about volatility, but if they plan to make systematic withdrawals for retirement, you need to know the effect of this volatility.
Let’s go back to the same chart again. Below, we have added a red line that represents the starting point of the S&P 500 Index on January 3, 2000, which was the first trading day of the year. What may surprise you is this: Over more than 13 years, the S&P 500 has spent less than 23.8% of the time above the red line and about 76.2% of the time below the red line. See Chart 2 on page 32.
S&P 500 Index from March 20, 2000 to August 1, 2013
For many years, the investment community told clients that they could withdraw 4% of their money annually without running out. But new studies have found problems with this approach. In fact, the Wall Street Journal recently ran an article titled, “Say Goodbye to the 4% Rule.” The Journal correctly identified the negative effect of volatility on a retirement account when a person makes predictable systematic withdrawals.
Our own study reveals some sobering information. We took a hypothetical example of a 65-year old man with $100,000. He plans to withdraw $4,000 per year, which is 4% of the current value. This works out to a monthly withdrawal of $333.33 to supplement retirement income over the next 13 years.
We tied his $100,000 to the monthly movements of the S&P 500 Index (excluding dividends) and began making the monthly withdrawals. By age 78, he withdraws $55,000. His current remaining value is $43,900. So over more than 13 years (164 months), he has a total combined value of only $98,900. Here’s the math: $54,000 in cumulative withdrawals + $43,900 in remaining account value = $98,900. So, even though the market was up overall, he actually lost money because of market volatility.
The hypothetical Chart 3, above, -illustrates how volatility affects our 65-year old client. He places $100,000 into an investment that tracks the S&P 500 index (excluding dividends) while withdrawing $4,000 (or 4% of their beginning balance.) He withdraws $333.33 per month from January 3, 2000 to June 2, 2013. (Please note that January 3 and June 2 are used because these are the first trading days of each month. The first trading day has been used to set a closing index price.)
So after 13 years and eight months, the total value came to just $98,900 even though he started with $100,000. Wouldn’t a CD or savings account have fared better? If he simply saved his money in the bank and earned just 1% with no volatility over that same period, he would have experienced the following.
• $55,000 in cumulative withdrawals.
• + $55,991 in remaining account value.
• $110,991 in total combined value.
Amazingly, the 1% bank product would have beaten the S&P 500 Indexed example above by $12,091. That’s a 12.25% better performance! It’s time to consider some alternatives.
MYGAs
The Wall Street Journal article recommends that people look into annuities as a solution. Today’s multi-year guarantee annuities can provide internal rates of up to 2.70% or better.
Immediate Annuities
Lifetime immediate income annuities can pay out a cash flow of 6% or more with a guarantee that people will never run out of money.
FIAs
Consider a fixed indexed annuity for people who buy and hold. Rather than riding the market roller coaster, consider a financial strategy that participates in S&P 500 Index gains when the index rises, but not when the index falls. This means that their money will grow or stay the same each year. Your client will not lose a penny related to changes in the S&P 500 index.
Get a Bonus
Some fixed annuities offer substantial up-front bonuses on their money. These can be as high as 10% of their deposit. That means a $100,000 deposit could be worth $110,000 from day one. Talk about getting a head start!
Tax Deferral
Another great benefit is that the interest your client earns on the annuity is not taxed until they withdraw the money. For a client who plans on long-term growth, this tax deferral allows their money to work harder; they continue to earn interest on the money that they would otherwise have paid in taxes.
Not All Annuities Are Created Equal!
As a professional advisor, you must work with your clients to make the process easy for them. Nationally, there are thousands of different annuity types; many designed to accomplish specific goals. To truly help people, ask them to allow you to perform a complimentary suitability review. Before making any financial recommendations, sit down together; evaluate their personal situation; and match their needs to the right product that was designed for that purpose.
Leave volatility and low yields in the past! Give the assurance of good planning and lifetime income today.
––––––––
W. Andrew Unkefer is president Unkefer & Associates in Glendale, Ariz. For more information, email andy@unkefermail.com or call 800-523-5851.
Dental Judgement Day – Get Help with the Tall Order of Deciding on Dental Plans with our Annual Survey!
Welcome to Part III of California Broker’s 2013 Dental Survey. We’ve asked the top dental providers in California to answer 28 crucial questions to better help you, the agent, understand their benefits, features, and services. Read the responses and sell accordingly.
19. If covered, explain the process that allows the general dentist to refer to the specialist.
Aetna: For DMO plans, general practitioners can refer to a participating specialist directly based on published guidelines. DMO members have direct access to participating orthodontists and do not need a specialty referral. Indemnity and PPO plans have direct access for specialty services.
Aflac: Aflac Dental does not require referrals.
Anthem Blue Cross: With our Dental Prime and Dental Complete plans, we do not require referrals. For the Dental Net DHMO, referrals that do not include high-risk procedures are reviewed post-treatment. Using the Direct Referral program, the participating general dentist can refer a patient to a specialist without prior authorization. Dentists’ practice patterns are reviewed to help ensure that they share in our commitment to providing access to effective healthcare. For the Dental Net DHMO products, the member’s assigned general dentist can call the customer service hotline in an emergency to get an immediate authorization for emergency services.
BEN-E-LECT: Referral is not necessary for any of BEN-E-LECT’s plans. The member may select a specialist and schedule an appointment upon making a phone call or personal visit.
BEST Life: No referral is necessary. Insureds can visit a specialist at any time.
Blue Shield: For DHMO plan members, the general dentist completes a specialty care referral form and provides a copy to the member, who provides the form to the participating specialist at the time of the appointment. Dental PPO plan members may self-refer to a specialist.
California Dental Network: A general dentist will determine if a member is in need of a specialty procedure that is not within his/her scope of practice. The General Dentist then submits a referral request to the Plan. The Plan Dental Director then determines if the procedure is dentally necessary.
Cigna: DHMO — Network general dentists initiate patient referrals for endodontic, oral surgery, and periodontal treatment. Referrals are confirmed for 90 days from the approval date. Specialty referrals are not required for orthodontic treatment or pediatric care for children up to seven years old, as long as members visit network specialists. The network specialist may submit a request for preauthorization to Cigna for oral surgery and periodontal services. Members are responsible for the applicable patient charges listed on the patient charge schedule (PCS) for covered procedures. After specialty treatment is finished, the member should return to the network general dentist for care.
DPPO — There is no need for a referral by a primary care dentist to obtain services from a specialist with the Cigna DPPO plan. Members may choose to seek service from any in- or out-of-network specialist or general dentist at any time. DEPO — There is no need for a referral by a primary care dentist to obtain services from a specialist with the Cigna DEPO plan. Members can visit any network specialist or general dentist at any time to receive coverage. Indemnity — Cigna Traditional indemnity members are always free to seek care from any licensed dentist at any time.
Delta Dental: Fee-for-service enrollees can self-refer; referral by the general dentist isn’t required. For DHMO enrollees, the primary care dentist is responsible for submitting the predetermination request and directing the enrollee to the appropriate specialist once authorization is received.
Dental Health Services: The general dental office sends Dental Health Services a specialist referral authorization. Upon approval, the authorization is sent back to the general dentist who informs the patient that they are now eligible to get appropriate care from a specialist
Guardian: For the DHMO plan, any complex treatment requiring the skills of a dental specialist may be referred to a Participating Specialist Dentist. Our DHMO plans offer Direct Referral in which the member may be referred directly by their primary care dentist to a participating specialist without pre-authorization.
Health Net Dental: For DHMO plans that require pre-authorization, the contracting primary care dentist completes a specialty referral form and submits to Health Net Dental. Approvals are returned to the primary care dentist, member and specialist. Upon receiving the approval, the member contacts the specialty office to schedule an appointment for completion of treatment. For plans that have direct referral, the primary care dentist may directly refer the member to a participating specialist by visiting our website or by contacting our customer service. Our PPO dental plans allow self-referrals to participating or non-participating specialists as needed.
HumanaDental: General dentists are encouraged to refer members to participating specialists to provide the highest level of benefit to the member. The general dentist can refer out-of-network if there are no specialists within a reasonable distance.
MetLife: Our Dental PPO product does not require referrals for specialist care. For Dental HMO/Managed Care, the SGX and MET series of Dental benefit plans allow participating general dentists the flexibility to refer members to participating specialists without prior approval – except for orthodontic and pedodontic specialty services in CA where the member’s selected general dentist will contact us for pre-approval.
Principal Financial Group: Patients can choose any provider in the network; referrals are not required.
Securian Dental: No referral is required.
United Concordia: If a general dentist determines that a patient requires referral to a specialist, all care must be coordinated through the primary dental office. The primary dental office should refer the patient to a participating specialist located in our Concordia Plus Specialist Directory and also complete the Specialty Care Referral Form. The patient should be given a copy of the referral form to give to the specialist at the time of their appointment. The specialist will then be responsible to submit the claim, corresponding documentation and referral form to United Concordia for reimbursement.
Western Dental: Once the general dentist determines that the necessary procedure is out of his or her scope of practice, the office will submit a written referral request to our plan. Western Dental’s dental director then determines whether the referral is medically necessary and whether the procedure is covered under the benefit plan.
20. Are any of your specialists board eligible/certified?
Aetna: Yes
Anthem Blue Cross: All contracted specialists with Anthem Blue Cross must be board certified/board eligible.
Aflac: For benefits to be payable, the specialist must be licensed by his or her state to perform the required treatment.
BEN-E-LECT: Yes. BEN-E-LECT requires that all participating specialists be board certified.
BEST Life: All of our specialists are certified and must meet a rigorous credentialing process to be admitted into the network. DenteMax credentials its specialists using the following elements:
• License to Practice
• DEA/CDS Certificates
• Education/Board Certification
• Work History
• Malpractice Claims History
• Malpractice Insurance
• Application and Attestation Content
• Sanctions Against Licensure
• Medicare / Medicaid Sanctions
• Medicare Opt Out
Our network dentists will be credentialed upon requesting participation in the network, and will be recredentialed no less than every thirty-six months.
Blue Shield: Yes, while this varies by specialist. Dental specialists may be certified, but it is not an industry requirement. Therefore we do not track board certification. We ensure that members receive the best possible care by credentialing and re-credentialing dentists following NCQA guidelines.
California Dental Network: Yes.
Cigna: DHMO/DEPO/DPPO — Every network specialist must certify that they have successfully completed post-graduate dental specialty programs in their fields. Our networks include specialists in periodontics, orthodontics, endodontics, pediatric dentistry, and oral surgery. Indemnity –Network related issues are not applicable to the Cigna traditional indemnity plan. Members may choose any licensed dentist to provide care.
Delta Dental: Delta Dental requires board certification where it is required by state law. Under the fee-for-service plans, Delta Dental credentials all of its participating specialists in the same manner, whether they are board-eligible or board-certified. Under the DHMO plans, Delta Dental requires all DeltaCare USA network specialists to be board-qualified.
Dental Health Services: Yes, the majority of our dental specialists are board certified.
Guardian: Many of our PPO specialists are board certified or eligible and all of the DHMO specialists are board eligible.
Health Net Dental: Yes.
HumanaDental: All participating specialists must provide copies of their specialty licenses or residency certificates.
MetLife: In order to participate with the Dental PPO or HMO/Managed Care, specialists must submit and keep current any certifications and/or other factors necessary to maintain their specialty.
Principal Financial Group: Yes. All specialists are required to be board eligible, board certified or be a designated specialist by the ADA.
Securian Dental: 100% of the specialists in our network are board certified or board eligible.
United Concordia: Yes, as part of our credentialing process, we verify each dentist’s education, license and certifications.
Western Dental: All contracted specialists are board-eligible/certified.
21. How do you fund your specialty care?
Aetna: Specialty services are paid on a fee-for-service basis.
Aflac: Aflac Dental insurance* pays a set amount per procedure based on a table of allowances. Additionally, policyholders have the freedom to choose their own provider without precertification. *Policies may not be available in all states. Benefits are determined by state and plan level selected. Refer to the policy for complete details, limitations, and exclusions. Coverage is underwritten by American Family Life Assurance Company of Columbus. In New York, coverage is underwritten by American Family Life Assurance Company of New York
Anthem Blue Cross: Claims for specialty care for both Dental PPO and DHMO plans are paid according to the provider’s fee schedule.
BEST Life: Specialty care is built into the premium. Specialty care received by a network provider is reimbursed at a discounted fixed fee schedule. Specialty care received by a non-network provider is reimbursed on what is usual and customary for that area, procedure and specialty.
Blue Shield: Specialty care is paid on a discounted fee for service basis for dental HMO, INO and PPO plan designs. Member and plan copayments vary, depending on the plan design.
California Dental Network: For plans that have specialty care coverage, the costs are built into the plans monthly premium rate.
Cigna: DHMO – We contract with an extensive network of specialists to ensure that our members are provided with the needed services at negotiated fee levels. Specialists are paid based on a reduced fee schedule. Patient charges listed on the patient charge schedule (PCS) apply at the specialist’s office once we have authorized payment. DEPO — The DEPO plan uses our national DPPO network. Specialists are part of the Cigna DPPO network, and members can seek care from any network specialist without a referral. DPPO — Specialists are part of the Cigna DPPO network; members can seek care from a network or non-network specialist without a referral. Indemnity — the Cigna Traditional indemnity plan is not a network-based plan.
Delta Dental: Specialty care is built into the premium. Under the fee-for-service plans, specialists are reimbursed by a combination of maximum plan allowances by procedure (contracted fees between Delta Dental and dentists) and coinsurance paid by the covered enrollee. Under the DHMO plan, network specialists are reimbursed for preauthorized services on a per-claim basis according to contracted fee schedule and copayment paid by the enrollee.
Dental Health Services: Specialty care and treatment are paid for on a contracted basis and payment varies by procedure. These costs are built into each plan’s monthly premium rate.
Guardian: Our PPO specialists are paid on a fee-for-service basis. For our
DHMO plans, specialty care is funded through a portion of premium.
Health Net Dental: For both our DHMO and DPPO plans, we underwrite and rate dental plans based on an assumed specialty care claims liability and build an allowance into our dental premiums.
HumanaDental: Specialists are paid on a fee-for-service basis according to a contracted fee-schedule amount or by reimbursement limit.
MetLife: For Dental PPO and HMO/Managed Care, specialists are reimbursed based on a predetermined fixed fee schedule. The SGX and MET Series of dental plans have co-payments and/or covered percentages for specialty services listed on the Schedule of Benefits for the plan.
Principal Financial Group: Through normal plan provisions.
Securian Dental: Network dentists (general and specialty dentists) are reimbursed on the basis of a discounted fixed fee schedule. Network dentists agree to accept the fee schedule amount as full consideration, less applicable deductibles, coinsurance and amounts exceeding the benefit maximums and will not balance bill the member.
United Concordia: For groups up to 149 employees, United Concordia actuarially create rates using client-specific demographics, including plan design, geographic location, prior carrier history, expected participation, and industry.
For groups with 150 or more employees, we use standard transfer business techniques to create group rates for new business and client-specific experience for existing business. As such, United Concordia requires claims experience when determining rates for clients with at least 150 enrolled contracts. United Concordia adjusts the prior carrier’s client-specific experience for assumed changes in-network utilization and payment levels, changes in benefits and utilization review, and projects it forward to the proposed policy period. We then add required administrative expenses and margins to create the required premium.
Western Dental: We incorporate into our premiums what we expect specialty care claims to be. We then pay the claims based on dental necessity and plan guidelines.
22. Does the member have to be referred by the primary dentist to the orthodontist or can he or she self-refer?
Aetna: Member can self-referred.
Aflac: Aflac Dental does not require referrals. Policyholders may self-refer.
Anthem Blue Cross: We do not require referrals in our PPO plans, including Dental Prime and Dental Complete. Members enrolled in the Anthem Blue Cross Dental Net DHMO program must be referred by their primary dentist to an orthodontist. Using our Direct Referral program, the participating general dentist can refer the patient directly to the specialist without prior authorization.
BEN-E-LECT: Members may self-refer to any orthodontist they prefer. In-network versus out-of-network and plan selection will determine coverage provided.
BEST Life: No referral is necessary.
Blue Shield: For dental HMO plans, the general dentist completes a specialty care referral form and provides a copy to the member, who brings this to the participating specialist at the time of the appointment. Dental PPO/INO plan members may self refer.
Cigna: DHMO — Specialty referrals are not required for orthodontic treatment or pediatric care for children up to seven years old, as long as members visit network specialists. The network specialist may submit a request for preauthorization to Cigna for oral surgery, endodontic, and periodontal services. DPPO — There is no need for a referral by a primary care dentist to obtain services from a specialist with the Cigna DPPO plan. Members may choose to seek service from any in- or out-of-network specialist or general dentist at any time. DEPO — There is no need for a referral by a primary care dentist to obtain services from a specialist with the Cigna DEPO plan. Members can visit any network specialist or general dentist at any time to receive coverage. Indemnity — Cigna Traditional indemnity members are always free to seek care from any licensed dentist at any time.
California Dental Network: For tracking and quality review purposes the Plan prefers that the primary dentist refer through the Plan. However, members may self refer.
Delta Dental: Under the fee-for-service plans, enrollees can self-refer. For DHMO plans, the assigned network dentist submits a referral request for orthodontic treatment to Delta Dental. The network dentist is notified upon approval and is responsible for advising the DeltaCare USA enrollee who then contacts the assigned network orthodontist for an appointment.
Dental Health Services: Yes, members must get a referral from one of our network dentists before visiting a participating orthodontist.
Guardian: PPO members can self-refer to all types of specialty care, including orthodontia. General Dentists in our DHMO network will refer the member to a Participating Orthodontist. The referral does not require plan authorization.
Health Net Dental: Our DPPO product does not require referrals for specialty or orthodontic care, so participants may self-refer. For DHMO, there are three types of specialty referral processes based on the member’s schedule of benefits. For plans that require pre-authorization, a specialty referral form must be submitted by the primary care dentist. For plans that have direct referral, the primary care dentist may directly refer the member to a participating orthodontist by visiting our website or by contacting our customer service. For plans that allow self-referral, the member may go directly to a contracted specialist by visiting our website or by contacting our customer service.
HumanaDental: In our PPO, the member can self-refer to an orthodontist. HumanaDental encourages members to ensure any dental provider is in-network. Humana has a provider directory available on our website, www.Humana.com. Members can also call the customer service number on the back of their insurance card.
MetLife: Our Dental PPO product does not require referrals for specialty or orthodontic care, so participants can self-refer. For Dental HMO/Managed Care in CA, orthodontic specialty services require pre-approval. The member’s general dentist will contact us for pre-approval, and once approved will contact the member with the name of a participating orthodontist.
Principal Financial Group: A member can choose to seek services from any provider.
Securian Dental: The member can self-refer.
United Concordia: Our PPO plans allow members to self-refer. Under our DHMO plans, the primary dentist determines if a specialty referral is required, regardless of the specialty.
Western Dental: The member has to be referred by the primary dentist to the orthodontist for our IPA Dental Plan. Our Western Centers-only plan allows the member to self-refer.
23. What is the time frame for processing a referral in terms of member notification and payment to the specialist?
Aetna: DMO general practitioners usually provide a member with an immediate referral specialty payments are made on receipt and adjudication of the claim.
Aflac: Aflac Dental does not require referrals because policyholders have the freedom to choose their own dentist without restriction.
Anthem Blue Cross: With our PPO plans, there is no need for a referral. With Anthem Blue Cross Dental Net DHMO plans, referrals are usually processed within 48 hours through the use of our Direct Referral program. Referrals for emergency reasons are usually processed within the same day.
BEN-E-LECT: Referral is not necessary. Members may call and schedule the appointment as desired.
BEST Life: No referrals are required. Members may self-refer to any specialist they choose.
Blue Shield: For dental HMO plans, the general dentist completes a specialty care referral form and provides a copy to the member, who brings this to the participating specialist at the time of the appointment. Our average turnaround time for claims payment to the specialist after receipt of the claim is approximately six days. Our dental PPO plans do not require referrals.
California Dental Network: Referral authorizations must be processes within 5 working days of receipt from the provider. Emergency referrals are processed immediately. Payment to the specialist is made within 30 days of receipt of a complete claim, often significantly faster.
Cigna: Not Available.
Delta Dental: For PPO and Premier patients, specialty care referrals are not required, and payments to specialists are processed the same as for general dentists. For DHMO enrollees, preauthorizations for specialty care are processed within five business days.
Dental Health Services: Emergency referrals are processed immediately. In a non-emergency situation, referrals are processed within one to two weeks. Claims are paid within two to three weeks.
Guardian: Referrals are not required under our PPO plans. For our DHMO plans, payment to the specialist is within 30 days of receipt of the claim.
Health Net Dental: The average turnaround time in processing a non-emergency referral is 48 hours and then 7-10 business days for the EOB to be received by the member.
Once the claim is submitted by the specialist, our average turnaround time in processing is 10 business days of receipt and then 7-10 business days for specialists to receive payment in the mail. If claim was sent electronically, it will be sooner.
HumanaDental: Most HumanaDental plans do not require a referral from a general dentist to a specialist. The member gets a higher benefit when seeing a participating dentist and specialist. In 2012, 96% of claims were processed within 14 calendar days
MetLife: For Dental HMO/Managed Care, standard referrals are processed in an average of five business days for member notification and 14 business days for payment to the provider. Our Dental PPO product does not require referrals for specialty or orthodontic care.
Principal Financial Group: N/A
Securian Dental: No referral is required.
United Concordia: All referrals are immediately effective. The member is instructed to provide the referral to the specialist at the time of service and the specialist files the referral with the claim. All claims, including specialist claims, mailed to United Concordia are usually processed within 14 days. Claims filed electronically are prioritized and processed accordingly with payment rendered during the weekly check writer cycle.
Western Dental: Emergency referrals are handled within 24-hours. The turnaround for non-emergency referrals is three business days. Specialists can expect payment in 10 business days for clean claims.
24. If you limit services with an annual or lifetime maximum, what does the maximum dollar amount allowed refer to?
Aetna: The maximum dollar amount refers to the total amount Aetna will pay for covered benefits.
Aflac: The annual maximum refers to the maximum amount of benefits that may be received within a policy year per covered person. Annual maximums do not apply to wellness and X-ray benefits.
Anthem Blue Cross: Our Dental PPO plans have an annual maximum, which refers to the maximum dollar amount that will be paid by the plan in a calendar year. With Anthem Blue Cross Dental Net and Dental Select DHMO plans, there are no annual or lifetime maximums
BEN-E-LECT: The maximum dollar and lifetime maximum refers to all services and procedures unless specified otherwise by benefit.
BEST Life: Lifetime maximum applies to orthodontia benefits. We offer multiple choices of calendar year maximums for preventive, basic and major procedures.
Blue Shield: The “maximum” is the maximum amount paid for covered benefits under the plan. The dental HMO plans have no annual maximum or lifetime maximum.
Dental PPO annual plan maximums range from $1,000 to $2,000 and encompass all dental services received except orthodontics. Dental INO plans have a $2500 annual maximum. There are no lifetime maximums for dental PPO/INO plans.
Orthodontia is offered to adults and children in many dental PPO plans as an additional benefit, which does not apply to the plan annual maximum. Group dental PPO/INO plans provide a generous calendar year orthodontic maximum of $1,000; there is no lifetime orthodontic maximum. Individual and family dental PPO plans offer low copayment and a two-year lifetime orthodonture benefit. Dental HMO plans have no annual maximum.
California Dental Network: For the DHMO, there is no annual or life time maximum for general dentistry care. Specialty care maximums vary by plan design and are separately explained in each plan’s benefit schedule. The maximum does not limit access to negotiated fees for covered services after the maximum is reached.
Cigna: For DHMO: There is no annual or lifetime maximum. For DPPO/DEPO/Dental indemnity: The maximum dollar amount refers to the maximum amount payable by Cigna for covered services rendered. Each plan design can be set-up with varying maximum dollar amounts.
Delta Dental: Under the fee-for-service plans, the maximum dollar amount refers to the maximum dollar amount paid by the plan. Our DHMO plans do not have annual or lifetime maximums.
Dental Health Services: The majority of our prepaid plan offerings have no annual dollar maximums, although this option is available by client request. PPO plan annual maximums range from $500 to $2,000.
Guardian: The maximum refers to the total of benefit dollars actually paid for covered services incurred within the annual period, or the member’s lifetime in the case of orthodontia. With Preventive Advantage, only Basic and Major services count toward the annual maximum. We also offer an option to cover cleaning after the maximum is reached.
Health Net Dental: The maximum dollar amount is the total amount the plan will pay for covered benefits.
Humana Dental: Annual maximum refers to the maximum amount paid annually for services, excluding orthodontia. Orthodontic treatment has a lifetime maximum
MetLife: For Dental PPO, maximums affect only the total annual reimbursement amount available under a plan to an individual or family. It does not limit access to our negotiated fees for services after the maximum is exceeded.
• For Dental HMO/Managed Care, there are no calendar or lifetime maximums.
• Negotiated fees for non-covered services may not apply in all states.
Principal Financial Group: The maximum dollar amount refers to benefits paid.
Securian Dental: The annual and lifetime maximum refer to the maximum dollar amounts we will pay for covered services in a calendar year (annual maximum) or over the coverage lifetime (lifetime maximum). Our plans generally include an annual maximum for non-orthodontic covered services and a separate lifetime maximum for orthodontia.
United Concordia: DHMO plans do not have annual or lifetime maximums. PPO plan annual and lifetime maximums vary by benefit plan and refer to the total amount paid in benefits by United Concordia annually or over the member’s lifetime.
Western Dental: The Series 7 DMO plans do not have an annual or lifetime maximum.
25. How and when do you provide eligibility information to your dental offices? How can you ensure that your offices will provide services to a member if they are not on the eligibility listing and it is after regular plan hours?
Aetna: Eligibility is available to our providers 24/7 by calling our automated telephone inquiry system or by accessing the online eligibility roster. DMO providers receive eligibility rosters the first week of each month.
Aflac: Providers may verify eligibility online – aflac.com – or by calling Aflac’s Customer Service Center – 1.800.99.AFLAC. Aflac Dental does not require prequalification for treatment.
Anthem Blue Cross: Participating providers can confirm eligibility via our secure website 24/7. Also, our customer service representatives are available toll-free Monday through Friday from 5:00 a.m. to 5:00 p.m. (PST) to help members with locating network providers, verifying provider status, member eligibility, answering claim questions, quoting plan benefits, and receiving member complaints. An interactive voice response (IVR) system is also available to answer calls and provide information 24 hours a day, seven days a week.
BEN-E-LECT: BEN-E-LECT provides electronic eligibility 24/7 through our Empowr web portal for providers and members. The Pre-Paid product will provide services upon collecting information from the member. This information will be transferred to BEN-E-LECT’s system electronically.
BEST Life: Providers can use our fax back eligibility system to determine if a member is eligible, outside of normal business hours. Offices routinely check eligibility prior to appointments and have a process in place for dealing with emergency situations.
Blue Shield: Eligibility lists for dental HMO plans are distributed to the dental HMO dental center during the first week of each month. Providers are responsible for contacting our Customer Service Department to verify eligibility, if a member is not on their list. Our Interactive Voice Response (IVR) is available 24 hours, seven days a week and has the capability to verify eligibility and assign members.
California Dental Network: Eligibility is available to CDN providers via Member Services 5 days a week. Providers also receive a monthly eligibility roster. The plan’s Website provides 24/7 eligibility.
Cigna: Members and dental offices can call 1-800-Cigna24 for access to our automated eligibility system, which is updated daily. In addition, an eligibility list is mailed to each network general dental office monthly for the Cigna DHMO plan. If no information is available for an individual who has identified him or herself as being covered, we will instruct the member to contact his benefits office for assistance.
Delta Dental: Dental offices can verify eligibility by contacting Delta Dental via our website, calling our automated information line or speaking with a customer service representative. Under the fee-for-service plans, a patient who is not shown as eligible may be asked to pay the entire amount of the bill up front. The dental office would be responsible for refunding the patient their overpayment after receiving Delta Dental payment. Under the DHMO plans, in addition to verifying eligibility as listed above, network dentists also receive eligibility lists at the beginning of each month. If an enrollee is not contained in Delta Dental’s eligibility database and claims to be eligible for benefits, Delta Dental contacts the client or the client’s benefit administrator to verify eligibility. If the eligibility verification is for an enrollee who has urgent or emergency needs, our customer service representatives will extend an urgent care authorization.
Dental Health Services: Participating dental offices receive eligibility rosters twice a month. If immediate eligibility is needed at any time, the dental office can call our 24-hour automated eligibility verification system or check eligibility online through our website.
Guardian: We do not provide eligibility lists for the PPO plan. Dentists can use our online self-service website, GuardianAnytime.com or call our toll-free line and receive a faxed verification of benefits from 3:00 a.m. to 8:00 p.m., Monday through Friday and from 3:00 a.m. to 1:00 p.m. on Saturday, Pacific Time. Eligibility Rosters for the DHMO plan are provided to the offices twice a month, at the first of the month and the 10th of the month. Dental Offices may also call our Member Services Department from 8:00a.m. to 5:00p.m. Monday through Friday.
Health Net Dental: Our DHMO dentists receive a monthly updated eligibility list that includes member name, member status (active, dropped, suspended or transferred), member ID number, dependent names and eligibility status, fee schedule code, group number and capitation amount, if applicable.
DPPO dentists do not receive an eligibility roster as members are not required to select a primary care general dentist. Members would simply choose any network dentist (or non-participating dentist, if they desire) and schedule an appointment.
DPPO and DHMO dentists can verify eligibility information via our interactive voice response system and Web site, which are both accessible 24-hours a day, seven days a week. Because the IVR and Web site are available 24/7, eligibility can be verified anytime of the day regardless of whether the need occurs during business hours.
HumanaDental: Participating offices are encouraged to check eligibility before providing treatment. They can verify members and benefits by calling our toll-free customer service line or through our automated information line to get 24 hour-a-day, seven-day-a week eligibility verification. There are no eligibility rosters for PPO business.
MetLife: For Dental PPO and Dental HMO/Managed Care, MetLife has developed a multi-channel technology platform for customer service inquiries including Web, fax, or phone. Through dedicated, real-time* channels, dentists have access to the same plan information provided to employees at the time of service. Dental offices do have access to dedicated online and automated phone system benefit information services to verify eligibility and plan details at any time. Additionally, Dental HMO/Managed Care eligibility data is forwarded once a month to each participating dentist. Transactions are processed in real-time except when the systems are undergoing scheduled or unscheduled maintenance or interruption.
Principal Financial Group: N/A
Securian Dental: Dental offices can use a toll-free number to call customer service to verify eligibility and benefits. Dental offices can also access www.securiandental.com to verify eligibility.
United Concordia: Dentists receive monthly capitation (eligibility) reports to verify DHMO members’ eligibility. They can also access member eligibility and benefit information 24 hours a day, 7 days a week through My Patients’ Benefits available online at UnitedConcordia.com or by using United Concordia’s IVR system, which can be accessed by dialing our toll-free Dental Customer Service phone number at (800) 307-8514.
Western Dental: Western Dental provides eligibility listings to our Staff Model Offices electronically and printed eligibility listings to our IPA Providers. This information is updated on the 1st and 15th of each month. For members who are not on the eligibility listing, we offer guaranteed capitation to our network of providers.
26. How do you handle early termination of coverage when a member is still in the middle of orthodontic treatment?
Aetna: We stop issuing our quarterly payments when the member is no longer covered.
Aflac: Benefits will cease upon termination of coverage.
Anthem Blue Cross: While details vary by plan, with our Dental Prime and Dental Complete programs, benefit payment is pro-rated based on the services completed.
BEN-E-LECT: Payment for benefits will cease at the end of the month for which the termination became effective.
BEST Life: Coverage terminates at the end of the month in which a member is no longer eligible.
Blue Shield: Once the member’s coverage is terminated, the cost of treatment is the responsibility of the member.
California Dental Network: Members losing eligibility during treatment will be charged the treating Orthodontist’s usual and customary fees for any unfinished treatment.
Cigna: Coverage for orthodontic treatment, which was started before disenrollment from the dental plan will be extended to the end of the quarter or for 60 days after disenrollment, unless it was due to non-payment of premiums.
Our standard extension of coverage is 90 days; however, other arrangements can be made.
Delta Dental: Delta Dental’s obligation to pay toward orthodontic treatment terminates following the date the enrollee loses eligibility or upon termination of the client’s contract.
Dental Health Services: If a member’s coverage is terminated in the middle of orthodontic treatment, we encourage the member to participate in a COBRA individual plan that will allow the member to retain orthodontic benefits. If the member chooses not to maintain their coverage, the dental office can prorate any additional treatment fees. The member would then only be responsible for the prorated amount of the full treatment cost.
Guardian: When an orthodontic appliance is inserted prior to the PPO member’s effective date, we will cover a portion of treatment. Based on the original treatment plan, we determine the portion of charges incurred by the member prior to being covered by our plan and deduct them from the total charges. Our payment is based on the remaining charges. We limit what we consider of the proposed treatment plan to the shorter of the proposed length of treatment, or two years from the date the orthodontic treatment started. Also, we enforce the plan’s orthodontic benefit maximum by reducing the total benefit that Guardian would pay by the amount paid by the prior carrier, if applicable. If a member is undergoing orthodontic treatment and his or her Guardian coverage terminates, we pro-rate the benefit to cover only the time period during which coverage was in force. We do not extend benefits. Our DHMO agreement provides for the contracted orthodontist to complete treatment at the contracted patient charge on a number of our plans. As an additional contract rider we can allow for supplemental transfer coverage for orthodontia under our DHMO.
Health Net Dental: Upon termination of coverage, we will pay for orthodontic cases in progress on a prorated basis up to the last effective date of coverage. Benefits are no longer payable after the member terminates and are the responsibility of the member and/or the new dental carrier.
HumanaDental: HumanaDental will prorate to provide the appropriate amount given during the time the member was in the plan.
MetLife: For Dental PPO and HMO/Managed Care, benefit consideration for orthodontic treatment will cease within the month that coverage terminates unless the participant obtains continuation of coverage, in which case benefits would continue as long as coverage remains in effect.
Principal Financial Group: On individual terminations, some of our plans allow for extended benefits that provide one month of additional coverage.
Securian Dental: Benefits are paid based on the services received while the member was covered by Securian Dental.
United Concordia: The extension of orthodontic coverage for DHMO and PPO plans is 60 days if payments are being made monthly. However, if payments are being made on a quarterly basis, coverage will be extended to the end of the quarter in progress or 60 days, whichever is later.
Western Dental: Western Dental has designed a termination clause to protect the member. The member does not incur any additional fees for the early termination of a provider.
27. How do you handle the additional cost of OSHA required infection control in your participating offices?
Aetna: These costs are a part of doing business.
Aflac: Since Aflac Dental does not have network requirements, policyholders can choose any dentist without restriction. It is the responsibility of the each individual dentist to meet OSHA requirements.
Anthem Blue Cross: Our relationship with network providers is an independent contractor relationship. We are not involved with how participating dentists run their offices. We do not allow a participating network dentist to bill members or receive plan payment for infection control as those changes are not allowed to be billed separately from a contacted dentist. On our Dental HMO plans, our contracted providers cannot charge members for the additional cost of OSHA requirements. It is the responsibility of the participating offices to absorb the additional cost of these requirements.
BEN-E-LECT: This cost is maintained by each participating office. BEN-E-LECT is not responsible for the cost.
BEST Life: OSHA costs are the responsibility of the provider.
Blue Shield: There is no sterilization charge paid by the member on our dental PPO plans; any additional OSHA costs are incremental and included in the fees of the provider.
Cigna: All Network Dentists should follow Centers for Disease Control and Prevention, American Dental Association, Occupational Safety and Health Administration, and any applicable state recommendations for sterilization and/ or infection control. Cigna considers sterilization, infection control, tray/setup and the handling/disposal of biohazardous waste to be included as part of the delivery of dental services and patient care. Therefore, neither the member nor Cigna may be charged separately for these services.
Delta Dental: The cost is included in regular dental office overhead. Network dentists are not contractually allowed to charge Delta Dental or its enrollees a sterilization/infection control fee.
Guardian: Most dentists have incorporated the cost of Occupational Safety and Health Administration (OSHA) requirements into the fees for services and do not charge separately. If it is the office policy to charge separately for OSHA, we do not restrict or limit the fee as long as all patients, not just the PPO patients, are charged. Since there is no CDT/ADA code for OSHA, Guardian plans do not cover such charges. Also, we do not allow participating DHMO dental offices to charge additional fees for this.
Health Net Dental: OSHA-required infection control procedures are not eligible for payment. It is industry standard to implement OSHA compliant infection control standards for all equipment, facilities and staff without a standalone fee and/or reimbursement. For those dentists who do charge a separate fee, payment is the responsibility of the patient, although a Maximum Allowable Charge (MAC) is established.
HumanaDental: Most offices have incorporated the cost of OSHA required infection control in their overall service charges. These costs would be reflected in the data used to compile fee schedules. It’s not usually a separate billable expense.
MetLife: Most dentists include these charges as part of their general overhead expenses which, in turn, are part of the fees submitted to MetLife. We use these fees as the basis for reasonable and customary data and/or for determining Dental PPO or Dental HMO/Managed Care provider fee schedules, as appropriate.
Principal Financial Group: N/A
Securian Dental: The dentist must be in compliance with OSHA required standards including:
1. Meeting OSHA guidelines for hazardous material disposal including sharps.
2. Meeting all state and local requirements for safety and health. The participating office would absorb any costs associated with fulfilling this requirement.
United Concordia: Participating dental offices include sterilization costs in their service fees. In turn, United Concordia uses these fees to determine our maximum allowable charge (MAC) and fee schedules. Through a partnership with an outside vendor, we offer participating dental offices access to discounted sterilization monitoring services.
Western Dental: Western Dental handles the additional cost of infection control in its rates and does not charge a co-payment.
28. Do you provide utilization data to your clients and brokers?
Aetna: Yes.
Aflac: Since Aflac products are individually issued, this is not applicable.
Anthem Blue Cross: Yes, Anthem Blue Cross provides a complete standard utilization and reporting package.
BEN-E-LECT: Yes. All data is provided at plan renewal and may be provided throughout the year by request.
Blue Shield: Yes. This is available upon request for employer groups of 300 or more employees at renewal.
BEST Life: Yes, we provide utilization information for large groups.
California Dental Network: OSHA and infection control costs are the responsibility of the providers. The Plan will not permit providers to sub charge the members for either of these costs
Cigna: Yes. Cigna offers a wide range of dental plan coverages and features that meet the needs of existing and prospective clients. Dental utilization information was integrated into the consultative analytics platform in late 2011 to enable more flexible request parameters, a consistent look and feel to medical/pharmacy/other reporting and updated norm information. We generally provide a standard package of dental information reports quarterly or annually at no additional charge. There is a charge for standard reports produced more frequently and for optional reports. Cigna dental plans are offered by Cigna Health and Life Insurance Company, Cigna HealthCare of California, Inc. or their affiliates.
Delta Dental: Delta Dental provides standard utilization reports to clients and brokers on an annual basis upon request.
Dental Health Services: Yes, Dental Health Services provides a wide range of utilization reporting, including treatment access, specialty claims activity, and member service call activity on client or broker request.
Guardian: Our standard reports are available monthly, quarterly or annually, and include the following detail: (1) dental plan summary, (2) monthly claims review, (3) cost management, (4) top 25 CDT codes by paid amount, (5) top 25 CDT codes by frequency, (6) benefits category claims comparison, (7) network overview, (8) out-of-network submitted charge comparison, and (9) claims by membership type.
Health Net Dental: Yes, we will provide utilization data upon request for large groups.
HumanaDental: Yes, on request and within the boundaries permitted by HIPAA.
MetLife: For Dental PPO and HMO/Managed Care, brokers are provided utilization data, if requested, as part of a proposal situation. Clients have online access to their utilization data or can be provided upon request.
Principal Financial Group: Yes, based upon the request of the client and/or broker.
Securian Dental: Yes, we can provide this information to individually rated employer groups upon request.
United Concordia: Yes, utilization reporting is available to clients and brokers.
Western Dental: Yes, utilization data can be provided on request to clients and brokers for large accounts.
29. Company Contact Information:
Aflac
www.aflac.com/broker
888-861-0251 • email: brokerrelations@aflac.-com
Aetna
We have people available to talk with producers in a variety of locations: www.aetna.com/insurance-producer/producer-support.html
We also have a general switchboard: 860-273-0123.
BEN-E-LECT
Mailing Address:
P.O. Box 7809
Visalia CA 93290.
Physical Address:
5429 Avenida de los Robles, Suite A,
Visalia CA 93291
Website: www.benelect.com
Toll Free 888-886-7973 • Fax 559-733-2325.
BEST Life
800-237-8543 • Fax 949.553.0883
www.bestlife.com • email: info@bestlife.com
Blue Shield of California
Producer Services 800-559-5905
Member Services 888-800-2742
California Dental Network
23291 Mill Creek Drive, suite 101
Laguna Hills CA 92653
Telephone 949-830-1600
Fax 949-830-1655 • Toll Free: 877-4DENTAL
www.caldental.net
Delta Dental:
Northern California Sales Offices
email: ncasales@delta.org
100 First Street
San Francisco, CA 94105
Phone: 415-972-8300 Fax: 415-972-8466
11155 International Drive, M/S A2S
Rancho Cordova, CA 95670
Phone: 916-861-2409 Fax: 916-858-0327
30 East River Park Place West, Suite 410
Fresno, CA 93720
Phone: 559-433-3010 Fax: 559-433-3009
Southern California Sales Offices
scasales@delta.org
17871 Park Plaza Drive, Suite 200
Cerritos, CA 90703
Phone: 562-402-4040 Fax: 562-924-3172
1450 Frazee Road, Suite 200
San Diego, CA 92108
Phone: 619-683-2549 Fax: 619-542-0269
Dental Health Services Corporate Office
Contacts: Josh Nace
Maria Escorsia
3833 Atlantic Ave.
Long Beach, CA 90807
562-595-6000 Fax: 562-276-1211
email: jnace@dentalhealthservices.com
email: maria@dentalhealthservices.com
Website: www.dentalhealthservices.com
The Guardian Life Insurance Company of America
Joe Stefano, Director, All of Southern/Central California, Las Vegas & Arizona
jstefano@glic.com
Main Phone 800-662-6464
Direct Line 949-885.1720 Fax 949-453-9919
Rick Porterfield, director, San Francisco, Sacramento & North, including Oregon/Washington
Richard_porterfield@glic.com
415-490-4433 • Fax 415-828-1990
Metlife
David Heil, Regional director, Northern California
1255 Treat Blvd, Suite 450
Walnut Creek, CA 94597
925-658-1102 • email: dheil@metlife.com
Doug Gehr, Regional director, Southern California
5 Park Plaza , Suite 1900
Irvine, CA 92614
949-471-2312 • email: dgehr@metlie.com
The Principal Financial Group
711 High Street
Des Moines, IA 50392
www.principal.com
Theresa McConeghey, Assistant Vice President – Dental, Life, Vision Products
mcconeghey.theresa@principal.com
United Concordia
1-888-884-8224
www.UnitedConcordia.com
Travel Health Insurance: Protect More Than the Itinerary
by Brendan Sharkey
When Helen and Ray landed in Southern Spain for what was meant to be a relaxing and rejuvenating vacation, they were feeling confident that they had planned carefully enough to meet all the expectations for their trip. They had planned enough, but their trip did not go as expected.
Shortly after arrival, Ray got seriously ill and was rushed to the hospital with a life threatening condition. Despite her panic and fear, Helen found comfort in the fact that having purchased international travel health insurance ensured that she would not be alone as she navigated care for Ray in a country where the language and the medical system were foreign to her. As Helen explained it, “The urgent nature of the situation was quite frightening. I wasn’t sure how to best handle it. I called my travel health insurance plan to explain the situation and get some help and it was then that I realized how important having that insurance is.”
Like many of those traveling abroad with travel health insurance — whether for a leisure trip or expat assignment — Ray and Helen know that health care is more accessible and understandable when you have the expertise and experience of an international health insurance company on your side.
According to the Office of Travel & Tourism, more than 60 million Americans traveled internationally in 2012, representing an increase of 3.4% over 2011. And in a recent study conducted by PricewaterhouseCoopers (Talent Mobility 2020 Report), experts predict that global corporate and international assignments will increase 50% by 2020. With this rise in the numbers of leisure and business travelers, the need for reliable travel insurance — offering personal and financial protection — is increasing as well.
Consider the Need
Many international travelers do not have appropriate insurance protection. Government sponsored health programs such as Medicare almost never cover care received in a foreign country. Employer-sponsored health plans often limit overseas coverage to emergency care only (and the burden will be on the traveler to prove the validity of an emergency). And emergency medical evacuation is almost never covered. Even if you’re traveling on business, you may have significant gaps in your coverage.
Understand Foreign Practices
Obtaining healthcare in some parts of the world can be tricky. Some hospitals won’t provide any treatment or won’t allow a patient to be discharged until the hospital has received a guarantee of payment. Such guarantees are commonly provided by travel health insurers, in conjunction with assistance providers, but rarely by other insurers or managed care plans. This means travelers will have to pay in advance, perhaps as much as tens of thousands of dollars. Some travelers will assume they can put these charges on a credit card and sort it out later, however, for this to be an option, the hospital must accept foreign credit cards and the credit card must have a sufficient credit limit.
Secure Quality Care
In some situations, transportation to another area will be necessary in order to access higher quality medical care. Medical evacuations are tricky to arrange and there are some air ambulance providers who should be avoided because they don’t have a good reputation. However, most travel health insurance includes a medical assistance benefit, which is critical. It provides 24/7/365 access to a company that will arrange an evacuation with a creditable evacuation company—or, through their medical personnel, can help assure that the patient gets appropriate treatment locally. The assistance company will also be available to help with other travel related problems such as legal troubles, lost passports or credit cards, etc. Emergencies are rare but everyone should have a contingency plan.
Plan Carefully
Expats and travelers should check with their insurance company and establish what kind of coverage they have. If it is difficult to get a straight answer from the company, that alone should be a warning. Those without insurance in the U.S. should consider that they might need it more than ever when traveling and recognize that the coverage can be cheap — as little as $1.50 to $9 per day.
Assess the Coverage Available
There are two types of coverage that expats and international travelers should strongly consider:
Health/accident insurance: Typically referred to as “travel health insurance,” these policies pay for doctor and hospital bills, and sometimes dental care and medications. These plans can be written for short trips (one day to six months) and will supplement Medicare or a managed care plan. International health insurance can also be purchased as primary insurance for expats or someone relocating to another country for an extended period of time (six months or longer). These plans are comprehensive and include added features such as preventative services, acupuncture, chiropractic, maternity benefits and more.
Medical Evacuation: Evacuations can be expensive (as much as $100,000 or more from a remote location). In addition to the coverage, travelers will want assistance arranging an evacuation.
Consider Additional Concerns for Expats
Insurance regulators have historically encountered international health plans primarily in the form of surplus lines products. These plans are technically not health insurance policies. Recently more than 40 U.S. states have recently stepped up to approve the sale of a new health insurance plan geared to serve people with global health insurance needs. Benefits are available inside and outside of the United States with no limitation on time spent in any one location.
Surplus lines coverage is quite different than true health insurance. The plans are designed very differently with far reaching consequences. An individual’s personal health and financial security could hang in the balance. Consider these advantages for securing admitted health insurance:
Critical Protection
Through admitted health insurance, travelers are protected under U.S. insurance laws and oversight. U.S insurance laws are strict and have long favored the health care consumer. This means that policy language must meet the plain English definition. Policy wording, plan definitions, exclusions, state mandates for coverage, claims process, claims turnaround times, formal appeals process all must meet regulatory muster. Additionally, agents are covered under their E&O insurance policy when they sell admitted coverage.
Ongoing Coverage Rights
An admitted plan can be kept for a length of time even after an expat’s employment ends or their overseas assignment ceases. U.S. insurance laws have stepped up to ensure portability and renewability of coverage. This is designed so that people do not suddenly find themselves out of a job, back home and uninsurable.
Medical Provider Networks
Larger networks tend to be available in the United States with fewer billing issues for members. In addition, contracted doctors and hospitals are available in most locations. These providers are set up in many instances to bill the insurance company directly. Providers are profiled and contracted and members can review their biographical information.
Better Benefits
Admitted benefits tend to be broader and deeper with few waiting periods or low limits on medical conditions.
Offer Your Clients Protection
Encourage your clients to ensure their safety and financial protection through the purchase of travel health insurance. In case they have an emergency abroad, they will receive the best medical care and assistance. Helen was able to focus solely on providing Ray with comfort and support because as Helen explained, “The insurance carrier assigned a team of professionals to us who helped me with everything from coordinating treatment with the hospital, to medical reporting, to guaranteeing payment, to assisting with our travel arrangements back to the U.S. They even sent a lovely nurse with us to assist us all the way until we were safely home.”
––––––––
Brendan Sharkey is director of Individual Programs for HTH Worldwide/GeoBlue in Radnor, PA, and is frequently called upon to discuss the travel insurance landscape. His most recent contributions include The Wall Street Journal, USA Today, Consumer Reports Magazine, the Los Angeles Times and the Washington Post, among others. Brendan has a great number of partnerships in the online travel, benefit platform and search engine arena. An avid traveler, Brendan has lived in Scotland, Canada, and Australia and holds a Bachelor of Commerce (Marketing) from Griffith University in Australia. Contact bsharkey@geo-blue.com
Life Insurance–Understanding the Full Value of Life Insurance
by David Hayward, CLU, ChFC, FLMI
When consumers think of life insurance, several things may come to mind. Some realize the value and seek out adequate amounts of appropriately planned policies. They understand and appreciate the leverage that can be obtained between their assets and the ultimate death benefit.
They understand the value of the living benefits that are included with many of the policies being sold. They enjoy the tax-deferred nature of the cash value growth in their policies. However, these consumers are not the norm.
The more common view is that life insurance is a necessary evil. While they accept that it’s important to protect their family against a financial hardship due to an early death, they often see life insurance as too expensive and not needed at the current time. It can always be purchased in the future, and no healthy person thinks they will die tomorrow. Too many consumers that have this viewpoint and they are missing out on one of the best asset classes to help them achieve many of their financial goals.
This article explores the different types of policies that a consumer may choose from and their associated benefits.
There are three different classes of life insurance that a consumer can choose from: Term, Whole Life and Universal Life. Term policies can have a level premium or annually increasing premium structure and generally last for fixed periods of time. Whole life can be participating or non-participating. The universal life class has several varieties to choose from: no-lapse, general account, indexed and variable. There are hundreds of different life insurance companies and many of them offer multiple styles of policies in the same classification of product. With this many choices, it is easy to understand why the typical consumer is confused about life insurance and is not naturally compelled to take action to get a policy.
Term insurance is different than the other types of policies because there is no cash value in the policy. Premiums are only calculated to cover the mortality costs and operating expenses of the policy. For a given year, term insurance will always come in with the lowest premium for a new policy, but there are few benefits other than the death benefit. If a person chooses to not pay their premium or forgets to pay it, they lose their death benefit protection. If their health status changes, it may be difficult for them to start over with a new policy. If they can start over, the premiums will be at a higher cost. The cost of a term policy goes up each year as a person ages or dramatically increases after an initial levelized period ends. The main benefit of term insurance is its lower price, but it gets very expensive as a person ages and the premiums paid are never recoverable if death does not occur while the policy remains in force.
All other types of policies offer the death benefit protection, but also have cash value associated with the policy. Rather than paying the lowest possible amount for the coverage, the initial premium amount is greater so the policy builds up a reserve of value that is then depleted in the later years when the term costs are extremely high. This produces a level premium over the life of the policy rather than increasing each year. A consumer can also pay a greater amount than the calculated levelized lifetime premium cost to attempt to have the full death benefit protection for life with a shortened premium paying period.
They can also create a large cash reserve to be used for other purposes in the future. Note that there are limitations imposed by the government that limit how much one can fund into a policy and still keep the classification of a life insurance policy. The cash reserve growth is not reportable for income tax purposes, but accessing it in the future may result in a lower death benefit. Depleting all of the reserve prior to death may cause the policy to lapse and may create undesired taxable income.
Whole life policies offer a guaranteed fixed premium that is calculated by the insurance company. If the premiums are paid as scheduled, the death benefit and cash value reserve are guaranteed and will never be diminished due to a poor investment structure, changes to interest rates or other factors. Because the insurance company guarantees the full value, the premium is often higher than with other types of policy. A participating policy offers a dividend if the insurance company can invest the cash value reserve and it earns more than the guaranteed rates the premium assumptions were calculated under. A non-participating policy may offer a lower premium and does not receive any type of dividend.
No-lapse UL policies blend some of the features of term insurance and whole life. Unlike term insurance that has an increasing premium; no-lapse UL premiums have a planned level premium calculated by the issuing company assuming guaranteed charges like a whole life policy. However, the cash value reserve is very low or may not exist at all. The premium is level, often calculated based on the number of years the client wants to pay the premium and how long they want the death benefit to last, but is not required like whole life premiums. If a client misses a payment or is late with them, the guaranteed values are diminished, which could cause a policy to lapse before maturity.
All other types of universal life policies shift the investment risk of the reserve from the issuing company to the client. Rather than a guaranteed premium and guaranteed cash value, the premium and cash value is based on a market interest rate and the premium is chosen by the consumer — often with the assistance of the agent. The current market interest rate is typically known, but future changes to the rate will impact the policy positively or negatively.
In a general account UL policy, the insurance company invests the reserves in a portfolio of bonds, mortgages and other conservative asset classes. The return on the block of investments determines the interest rate credited to the policyholders reserve account. The current rate is often guaranteed for one year, and subsequent rates depend on the investment experience of the insurance company’s investment team. If the initial planned rate is higher than the future market rate, the policy may be underfunded and may not last the lifetime of the insured. If the future market rate is greater than the planned rate, the cash value may grow and be greater than planned. This could allow the client to stop premiums early or have their policy grow in value. Adjustments may be made to the premiums in the future as needed to bring the policy back towards the initial expectations.
In an index UL, the cash value reserve grows in value based on the growth of a specified external index. Part of the cash value reserve is set aside to cover the current year’s charges. The remaining value is guaranteed to remain level over the next year, but may earn interest. The insurance company uses part of the reserve to purchase options on the underlying index, which determines the interest rate that will be earned on the reserve account. If the change in the index values is negative over the stated holding period, no interest is earned and the reserve account value remains unchanged. If the index increases in value, the percentage change, or multiple of it, is the amount of interest that will be credited to the policy reserve subject to a maximum caped value.
Variable policies’ interest is determined by the performance of chosen sub accounts, which are selected by the client. Sub accounts are comprised of a group of stocks, bonds, or other assets. Variable products are sold through a registered representative of a broker-dealer and may not be suitable for all clients.
Regardless of the type of product chosen, life insurance products have several characteristics that may benefit clients in the future. For policies that have a cash value reserve, all interest that is earned grows income tax deferred. If a client wants to remove some of their reserve in the future, it can be returned to them income tax free if done properly through withdrawals or loans, provided it is not classified as a modified endowment. Any time a client chooses to remove some of the reserve balance, they will lower their net death benefit, which may cause a taxable event if the policy lapses.
At retirement time, many clients have their mortgage paid off; their children have finished school; and other financial changes may have happened. Their death benefit needs may not be as large as it was earlier, so some clients choose to reduce the amount of their death benefit and deplete the cash value reserve over their remaining lifetime to supplement their retirement income. There are even optional riders with some companies that can guarantee a level amount of income over the insured’s lifetime. Some choose to take one larger disbursement leaving enough reserve value to cover the anticipated reduced future death benefit costs to their life expectancy. Others wish to keep the full death benefit intact to create a legacy for their heirs. There are lots of options available for the future use of a person’s policy.
Another valuable benefit often associated with many types of life policies is having living benefits. If a client suffers a terminal, chronic, or critical illness, they may be able to accelerate a portion of their death benefit at a discounted value to be used immediately. If one of these unfortunate events happens, the medical and other related costs can be high and cause a burden on one’s finances. The policy value received is often the present value of the death benefit accelerated based on the client’s future life expectance. Since this is considered an advance of the death benefit, it is often received income tax free. Note that the rules may vary depending on the size of the acceleration, the way the money is used and the state the client resides in. Not all companies and products offer living benefits.
In the end, when death occurs, the death benefit payable to the beneficiaries is generally income tax free and can be used for any purpose the beneficiary chooses. It can also be paid into a trust so the insured can structure how they wish the proceeds to be used and disbursed.
There are a variety of reasons people choose to purchase life insurance. Determining the amount of coverage is often the hardest issue. Common desires are to have the death benefit pay off the mortgage in the event of an early death; complete the funding of the retirement account for the surviving spouse; cover children’s education costs; provide for an inheritance not relying on saving other assets; provide funds to care for a special needs child; and pay estate taxes, final expenses, debts, and other items at the time of death. There are also charitable and many business applications for the death benefit.
Most consumers don’t object to owning life insurance; they just don’t understand all the benefits it offers. It is the agent’s role to help their clients understand this value and help them structure an appropriate mix of products to meet their needs. There is often not just one policy that is needed; a combination of the different types may create the overall benefit that is desired. Term policies are less expensive and can cover short-term needs while permanent policies with a cash reserve help with the long-term needs. Client’s needs may change in the future, so it is always a good idea to have annual reviews and make adjustments as needed.
–––––––––
David Hayward, CLU, ChFC, FLMI, is an advanced sales consultant for National Life Group. He specializes in the family protection, retirement planning, and wealth transfer markets.
Hayward received his BSBA from Drake University with a major in insurance. Prior to joining National Life Group in 2008, he had worked with American General Life and Accident Insurance Company’s Mature Market division and the ING Group’s Educational Services and Advanced Marketing departments. Hayward can be reached at 802-229-3801 or dhayward@nationallife.com.
Individual Heath – The New World for IFP Agents with the Exchange & Tax Credits
Beginning October 1, consumers can shop for coverage in the Health Insurance Marketplace (Individual exchange) without the current non-guarantee issue and pre-existing condition stumbling block. Do your individual and family plan (IFP) clients, and previously declined applicants, understand that?
Employee benefit agents are preparing clients to notify their employees about the exchange option and the potential eligibility for a health tax credit (aka government subsidy, premium assistance). You, as an IFP agent, should imagine that your clients will be receiving a notice in more ways than one. And, not being certified to sell insurance through the exchange (Covered California) may leave the back door of retention wide open for your IFP block of business. Furthermore, there is an action plan to take within the turbulence implementing the Affordable Care Act (ACA). This will include expertise in at least three areas to service your exising and new client prospects in the new world: inside the exchange, outside the exchange, and Medi-Cal adult and children eligibility options. We still have many unanswered questions, but let this not prevent us from becoming experts in this new world of selling and servicing health insurance policies for individuals and families.
Inside the Exchange
First, the exchange option with the health tax credit may or may not be a compelling story for the uninsured and current IFP clients who don’t have an employer-sponsored health plan subsidizing all, or a portion, of their premiums.
The basic understanding of the exchange is a marketplace to shop for affordable, standardized benefit plans (Bronze, Silver, Gold, Platinum) with a potential health tax credit for applicants with a Federal Poverty Level (FPL) between 138% to 400%. This means that a single earning between $16,000 to $45,000 annually may qualify, and a family of four with an income of $33,000 to $94,000 may qualify as well. If your clients earn income under or over these amounts, you will have to help them navigate shopping outside the exchange as well as assiting in Medi-Cal eligibile enrollment for those applicants under 138% FPL.
It is possible that many of your clients with an IFP policy may not qualify for the health tax credit, but this is part of your action plan to help navigate your clients into 2014. You must start your clients with shopping the exchange and eligiblity to receive a health tax credit to purchase a lower cost plan with similar or better benefits than their current IFP policy.
In essence, the exchange is positioning itself parallel to the current employer’s role in subsidizing premiums for eligible full-time employees. This can be attractive for IFP clients if the cost for coverage in the exchange is less than their current cost.
Carriers will also be reaching out to your block of business and notifying them of the exchange option which will not be helpful if you aren’t certified in the exchange. Registration for training and certification begins this month.
Agent commission will remain a hot topic with confusion and gray areas in the calculation of commission for IFP policies sold within the exchange. In Covered California’s Board Recommendation Brief releasd May 13th, 2013, agent commissions were stated to be “market-rate” with commissions outside the individual exchange. This will become clearer as we approach October 1 with the release of rates and commission structures for plans sold outside the exchange. One of the noted commission understandings for policies sold within Covered California is the calculation for commission based off the total premium rate, even if the applicant chooses the Advance Premium Tax Credit (APTC) option, which lowers the monthly premium payment. Some argue that commissions will be paid off the amount paid by the member, but this hasn’t been communicated by Covered California.
To dig deeper on the commission calculation, your clients could pay the full monthly premium and take the health tax credit at the end of the year as a tax refund, which would make sense for the commission to be based off the full premium paid by the member, but market studies show the APTC option will be more attractive. And, if the APTC option has a lower commission calcualtion, this would be a conflict of interest for agents and not be perceived as “market-rate” commission. Keep in mind that the new IFP world will require understanding of how to deal with under and/or overprojecting annual income. Your IFP clients notify Covered California, which would change the APTC amount and monthly premium payment for the client, or wait until filing taxes to clean up any income miscalculations. At the end of the day, it’s important to note that it seems to be the case that you would be selling an IFP policy in which your client only pays $300 per month (with APTC applied), yet your commission is based on the total premium which may be $800, for example.
Outside The Exchange
Second, for your IFP clients who aren’t eligible for the health tax credit, or have an FPL percentage from 300% to over 400% it will be important to look and compare rates and benefits for health plans offered outside the exchange as well. With that being said, those over 300% FPL may also consider the option in the exchange to apply the health tax credit and buy-down to a more affordable Bronze Plan. Even though a client may be eligible for subsidy with a 350% FPL threshold, the plan benefits and/or provider networks outside the exchange may offer a more competitive option. Once rates and networks are released you will be able to begin comparing exchange plans against those offered outside the exchange.
Medi-Cal Eligibilitiy
Third, you should plan on becoming familiar with how to handle the new Medi-Cal eligiblity and enrollment process when it comes up for adults under the 138% FPL threshold, as well as the split family 250% FPL threshold. It’s been clear, for some time, that adults under 138% FPL would be eligible for Medi-Cal, but Covered California is now beginning to communicate the “split family” example where the parents would be eligible for the exchange plan option with a health tax credit, but the kids would be eligible for the new Medi-Cal Kids program. In this scenario, you can help the client look to find a health plan outside the exchange for the kids, but the premium may be unaffordable. This will be problematic in implementing individual exchange options for households under 250% of the FPL, but it is not insurmountable.
In conclusion, it’s worth taking a long hard look at this new world around the corner, and what actions steps need to be made in order to transition your current IFP block of business. A successful transition includes becoming certified to sell options inside Covered California’s Individual exchange. In addition, the core knowledge needed will be understanding how the health tax credit works with eligibility and APTC calculation along with enrollment for subsidy eligible applicants and non-subsidy eligible as well. We will soon see if the plans are in fact affordable both inside and outside the exchange, and begin to help our clients and new prospects in the pursuit of purchasing affordable health insurance.
––––––––––
Garrett Viggers has spent 11 years in the insurance industry as a broker, consultant, and CDH and ACA expert. He helped launch CDH company, Veritas Health Systems in 2002 and Inovious in 2006, a SaaS company. He recently launched the cross-platform Affordable Health App Silver Plan advance premium tax credit quoting tool for brokers across the country. The the iPad/Table ACA Tool kit is scheduled to be released soon. Viggers is president of Windfall App Technologies, a spin-off company from Inovious, which focuses on app solutions for the health insurance marketplace exchange. For more information, visit www.AffordableHealthApp.com or email garrett@windfallapps.com.
Voluntary Benefits – The Upside of Health Care Reform for Producers: Voluntary Benefits
by Adam Michaels
It seems that the news surrounding the Affordable Care Act (ACA) is changing almost daily. Though some elements of the regulatory requirements have been delayed and others may still be altered, there is no doubt that employers are digesting the available information and reviewing their options for offsetting the potential costs of complying with the new law.
What it All Means to Decision Makers and Their Employees
Although several aspects of the new law are already in effect and the timeline has been shifting of late, the majority of the ACA will more than likely be phased in over the next several years. And, as major medical insurers brace to absorb the financial impact associated with guaranteed issue, minimum loss ratios, the elimination of rescission and the like, employees and the employers should be diligent and anticipate the changes to their coverage that are sure to be on this not-so-distant horizon.
With premiums estimated to go up by as much as 64% to 146%, the biggest change in the future is going to come in the form of shifted risk. We already see an increasing number of employers moving to consumer-driven or high-deductible plans, passing not only more of the premium, but also increased deductibles and copayments that reflect those in the government plans.
Like it or not, employees will face more risk, more decisions, and more personal responsibility as ACA forces health care coverage to be redesigned. As employees and consumers on public exchanges take the driver’s seat, they will make choices that could have a major impact on personal finances. Unfortunately most consumers are completely unprepared. In fact, according to the 2013 Aflac WorkForces Report, 54% of employees surveyed said, “I would prefer not to be in more control over my health insurance expenses and options because I will not have the time or knowledge to effectively manage them.” What’s more, 72% of workers have never even heard the phrase “consumer-driven health care.”
Perhaps what is more disconcerting is a lack of financial preparedness by most Americans. In fact, while 49% of employees believe the number of health care services not covered by health insurance will increase, only 23% report increasing their savings to mitigate these potentially higher medical costs. In fact, 46% of consumer respondents say they have less than $1,000 in savings designated for medically related out-of-pocket expenses. A large share rely on credit cards as their default safety net while 36% say they would have to borrow money if faced with the typical out-of-pocket expenses that come with unexpected illnesses or injuries.
More than likely, employees who are receiving insurance for the first time, as well as employees who have long been covered by company sponsored plans, will be rudely awakened when they realize that their portion of a typical hospital visit will be accompanied by out-of-pocket costs ranging between $2,970 (platinum) and $5,080(bronze). The resulting financial woes will affect not only the employee, but also their employers who will feel the impact through lower employee morale, decreased job performance, absenteeism, and dissatisfaction.
Voluntary Benefits: More Relevant Than Ever
The solution to the highlighted issues may well be voluntary insurance policies, such as accident, hospital indemnity, critical illness, cancer and disability insurance plans. Producers are searching for ways to meet client needs. Solutions that don’t add budgetary costs have now become an imperative.
Well-versed producers position voluntary insurance as part of their overall strategy instead of as a footnote at the end of a proposal. This positioning answers the questions from HR professionals and decision-makers of how to soften the blow of the inevitable cost-shifting and rising out-of-pocket expenses on its valuable workforce. In doing so, these producers help their clients redefine benefit strategies while ensuring that they protect their investment against negative employee perceptions. In fact, statistics show that voluntary products help employers meet their bottom line by improving employee engagement and complementing an overall benefit strategy. According to the Aflac study, more workers who have access to voluntary products say they are extremely satisfied or very satisfied with their benefits compared to workers who do not have voluntary products (69% compared to 48%).
Decision-makers and producers have figured out that adding voluntary insurance products not only increases an employee’s perception of robust benefits, but also increases the likelihood that an employee can stay ahead of the direct and indirect expenses from an unexpected health event or injury.
––––––––
Adam Michaels is the California-Los Angeles state sales coordinator for Aflac. He is responsible for creating and implementing the state’s strategic market development plan as well as acquiring and training new talent for the sales force. For more information about Aflac, visit aflac.com or email adam_michaels@us.aflac.com.
Marketing – A New Marketing Plan for a New Market
by Joe Navarro
Today is an age of an increasingly connected, socially conscious, transparent culture. Consumers are evaluating what the transformation of the health care industry means to them. What we are all about to experience is an advertising/marketing/word of mouth Tsunami like we have never seen before, and health insurance will be center stage for months to come.
To assist you in being successful during the health care reform era, you need a clearly defined, clearly communicated purpose that you embody as an agency and project in your marketing.
We continue to experience shock waves as we prepare for open enrollment. Just as we think we have a better understanding of what our market will look like, we are informed of alterations. If you haven’t already done so, now is the time to develop and implement your marketing strategies to take advantage of all the opportunities (and there will be plenty) surfacing as a result of the reconstruction going on.
If you haven’t already started I offer you the following to help get you going:
Plan for Managed Chaos In General – Be Prepared For All Possibilities
Immediately make contact with every existing and former client, emphasizing that you are the source of knowledge when it comes to health care reform. Accept that there is probably too much to take on yourself and identify a reliable resource to provide answers to the many questions and provide marketing assistance. Save all of the most commonly asked questions and create a custom health care reform FAQ for your clients. Keep tabs on the marketing efforts of Covered California and carriers to know what they are marketing and where so you can participate in the discussion.
Granted it is confusing. Simplify what is available for your clients when they come calling. Keep tabs of what your clients are experiencing. Survey them. Keep your finger on their pulse.
Diversify Your Product Offerings; They Will Be Shopping
Clearly establish your point of difference and use it to market yourself. Change your message. Our industry is changing; new products are being introduced; the four generations in the workplace are uniquely stimulated. The old map is out the door.
Expand your Internet presence; push out information with your blog; and pull them back in with your Website.
The benefits of a planned marketing strategy are numerous. You can no longer rely on intuition to make business decisions; there is too much at stake. Be brilliant.
–––––––––
Joe Navarro is director of Marketing for Warner Pacific. He can be reached at 800-801-2300, ext. 452.
