 Life Insurance – Creating a Social Security Legacy Plan
Life Insurance – Creating a Social Security Legacy Plan
by John A. Davidson, LUTCF, FSS • Social Security is projected to run out of money by 2035. With permanent life insurance, you can explore new possibilities for your clients and create a more stable future for their family and future generations Health Reform
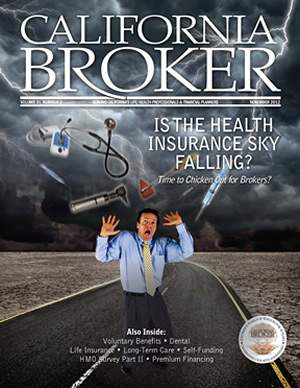
Health Insurance – Is the Health Insurance Sky Falling?
Time to Chicken Out for Brokers?
by Leila Morris • Industry experts who spoke at the SeeChange Health Broker Expo focused on seizing opportunities in the post-health reform market.
Exchanges Bring Big Opportunities for the Industry
By 2021, the exchange market is expected to more than double, marking the largest expansion of health coverage since the creation of Medicare in 1965
Dental–Diabetes Month Brings a Renewed Focus on Periodontal Disease
by Dr. James Bramson • During American Diabetes Month in November, it is important for you and your clients to know that periodontal treatment and ongoing maintenance can decrease the annual cost of medical care for people with diabetes.
Dental–A Good Dental Wellness Program in Your Portfolio Could Mean Increased Sales for You
by Timothy Custer, D.D.S. • When we think of dental problems, fillings, extractions, and root canals spring to mind. True, those are common and often costly. But, periodontal disease looms larger in prevalence and far-reaching detrimental effects than any of those.
Dental–A Case for Selling Dental Insurance to Small Companies
by Tom Morey • The demand from today’s workers is being heard loud and clear. Dental is the third most demanded benefit after major medical insurance and retirement benefits. So why aren’t some smaller employers offering it?
HMO Survey Part II – Retrieving Information on HMOs – Our Dogged Research Pays Off
Each year California Broker surveys health maintenance organizations (HMOs) in the state with direct questions about their plans. We then present the answers to such questions here for you—the professional agent or broker. We hope that this valuable information will help you serve your savvy healthcare clients better.
Self-Funding–Self Funding in 2013 with the Affordable Care Act
by Mark Reynolds, RHU • A little preparation now can catapult brokers into a new generation for their agency and they will see their business grow and thrive while many others sit and wonder. Brokers who adapt to a self-funded, solution-based marketing approach that actively markets for business can prosper while providing real solutions for employers.
Self Funding–Three Reasons to Stay Self-Funded Since the Affordable Care Act
by David Zanze • Make no bones about it; employers will spend more on healthcare expenses for employees. But self-funded employers will be better situated to control costs.
Long Term Care–How to Discuss Long-Term Care Insurance vs. Self-Insuring with Clients
by Steve Cain • It is clear that the long-term care insurance industry has struggled to increase market penetration for the masses. Part of the problem may be the way agents are positioning this issue. The effects of this sweeping healthcare legislation.
Premium Financing–Turning a Good Year Into a Great Year with Premium Financing
by Leila Morris • An agent may only sell two or three large life insurance cases in a year. So closing that one extra case can make the difference between having a good year and having a great year. Premium financing can tip the balance toward selling that large life insurance policy. Experts addressed premium financing opportunities at Succession Capital Allianceís fourth annual conference in Las Vegas in August. More than 100 advisors attended the two-day invitation-only event.
Voluntary Benefits–Going Green Just Got Easier for Employees
by Dominick Zenzola • Congested roads, smog, greenhouse gases – these are just some of the consequences as millions of people make their way to work each day in single-occupant, gasoline-powered automobiles. To encourage employees to use mass transit and reduce the impact on the environment, employers are allowed to offer federal tax-free commuter benefits. These benefits allow employees to reduce their monthly commuting expenses for mass transit, vanpools, and work-related parking costs.
Life Insurance – Creating a Social Security Legacy Plan
by John A. Davidson, LUTCF, FSS
Whether you are planning to retire soon or you are several years away from retirement, you have probably have seen the latest headlines about Social Security. Unless Congress acts soon, Social Security and the fund that helps finance benefits for 44 million senior citizens and survivors of deceased workers is projected to run out of money by 2035.
That’s three years sooner than anticipated, according to the Social Security Administration’s (SSA) trustees’ annual report. So we don’t have a moment to lose to enact some important changes that will affect millions of Americans.
This very serious topic of discussion opens up some great selling opportunities for making permanent life insurance and annuity sales to clients who are not likely to rely solely on Social Security to retire.
How can your clients plan for a secure income for their families amidst the uncertainty about the level of Social Security benefits that will be available in the future? They can leverage life insurance that is paid for with a portion of Social Security benefits. As politicians continue to discuss means – tested benefits, this issue has become more important for clients who don’t rely solely on Social Security, but have it as additional income. As the federal safety net comes under increased strain, your clients may need additional dollars for spouses, children, and grandchildren to continue in the lifestyle to which they’ve become accustomed.
Suppose your prospect is a 66-year-old man who doesn’t need the full monthly amount of his Social Security to live on. He may still be working. We can fund a permanent life insurance policy using $1,000 per month of his Social Security benefit. Upon his death, (provided sufficient premiums were paid), his beneficiary would get the full death benefit.
The surviving spouse has some great options to use money from the death benefit: invest it into an immediate annuity to provide income; put it into a trust to help ensure that adult children have retirement income in case the federal safety net fails; use it to pay off a mortgage; or use it for any other purpose the policy owner may have foreseen.
Also, because this is life insurance, policy proceeds are tax-free income. A tax-deferred cash-value accumulation can be accessed on a tax-preferred basis if needed. The client has flexibility to adjust planning needs moving forward.
In the scenario described above, the $1,000 monthly premium could provide more than a $500,000 death benefit and an internal rate of return of 5.24% on an after-tax basis (using a universal life insurance policy). This competes very favorably with other fixed income alternatives. However, keep in mind that, with universal life insurance, the premium amount that’s needed to keep the policy in force may fluctuate more or less than $1,000 per month depending on future interest rates and other factors. Whole life premiums are higher, but they do offer fixed premiums and stronger guarantees.
Simply repositioning some of the monthly Social Security benefit into the life insurance policy is a great way to create a safety net for your Social Security benefits.
Many seniors who remain employed after 65 find an alternative source of funds in the savings they get from purchasing a Medicare Supplement plan versus the high cost traditional health insurance coverage. The premium difference may be as much as $500 per month, per person. Of course, premium dollars could be found from ongoing wages, or other retirement assets.
Regardless of how the clients funds the new life insurance policy, as long as sufficient policy premiums are paid, the benefit can provide guaranteed income for his family without them being entirely dependent on the unstable Social Security system.
If the client’s wife uses the death benefit to get an immediate annuity, she could receive an additional $3,209 per month for the rest of her life (assuming age 80 and installment refund). This ensures that she will not outlive her assets and that the full purchase payment is made to an heir if she dies before it is paid out completely. This amount is greater than the original planned $1,000 monthly premium. It could easily be used to supplement existing federal benefits, offset reductions, or make up for a complete cessation of those benefits.
This permanent life insurance sales plan can be tailored to a variety of needs. In addition to being set up for a surviving spouse and children, it can be used to create a legacy trust for grandchildren to fund college tuition or other future needs.
Another great option is to use the life insurance to fund a charitable planning program for a favorite charity. Check with a tax advisor about the tax benefits of gifting this policy and funding the program for seven or 10 years.
A recent Gallup poll reveals that 57% of retirees say Social Security is their major source of income. With permanent life insurance, you can explore new possibilities for your clients and create a more stable future for their family and future generations.
–––––––––
John A. Davidson, LUTCF, FSS, has been associated with Ohio National since October of 2008 and is based in Thousand Oaks, Calif. John is past president of the San Fernando Valley Association of Insurance & Financial Advisors, past president of the California Association of Insurance & Financial Advisors and past president of the National Association of Insurance & Financial Advisors. He is also a member of the Society of Financial Service Professionals and a member of the Association for Advanced Life Underwriters. John is a 27-year Qualifying & Life and Court of the Table member of the Million Dollar Round Table. Davidson Insurance & Financial Services, Inc. can be reached at 805-495-6434.
Is the Health Insurance Sky Falling?
Time to Chicken Out for Brokers?
by Leila Morris
A July article in Forbes magazine warns, “The floodgates are about to open for the mass firing of healthcare insurance agents…There will be a huge migration of business from traditional healthcare insurance agents and brokers to the exchanges…similar to the migration of retail from…Borders to Amazon.com. At least in retail, there are numerous good reasons…to go to the brick and mortar stores…The argument for procurement through agents is very weak.” The writer, Nigam Arora, who describes himself as an engineer, nuclear physicist, and entrepreneur, goes on to sound the death knell for health insurance agents in two more articles in Forbes.
Is this physicist correct about the sky falling? Not if you talk to insurance industry experts who spoke at the SeeChange Health Broker Expo held September 19th to 20th in Las Vegas. The event didn’t focus on lamenting the passage of the Patient Protection and Affordable Care Act (PPACA) or worrying about the future, but on seizing opportunities in the post-health reform market.
Providing some market predictions at a panel conducted before the Expo officially began, were Warner Pacific’s Jeff Papenfus, senior vice president of sales, John Kurath, vice president of sales for Colorado, and Neil Crosby, director of sales. They stressed that employers are looking for brokers to educate them on health reform; offer solutions; and help with compliance issues. As he has said often in the past couple of years, Warner Pacific’s Co-CEO, John Nelson said that brokers will continue to be needed and valued in the post health reform market.
The individual plan market is expected to grow 100% to 300% with as many as 28 million new insureds by 2016. Sales are expected to double, if not triple. Fueling the growth are subsidies and guarantee-issue requirements. Carriers may have slashed commissions to comply with medical loss ratio (MLR) requirements, but individual plans will be much easier to sell when you don’t have to worry about applicants getting rejected because of preexisting conditions. Also, premiums on individual plans are expected to increase 30% to 50%.
What about group plans? Will the group market shrivel as employers drop coverage en mass and push workers toward exchanges? Nelson and others say no. In fact, a recent Mercer survey of employers finds that few plan to cancel their health benefit plans after reform is fully implemented. According to a PWC study (see page 16) many employers do not see dropping health benefits as a viable solution due to penalties, tax consequences, and their employees’ expectations of having health benefits.
There is no question that some employers will drop coverage, especially those with high concentrations of lower-wage workers who qualify for federal subsidies through the individual exchange markets, according to PWC. Nelson noted that, due to budget constraints, the federal government may make it harder for individuals to qualify for the subsidies.
Also, brokers will be selling through the exchange in California. Recognizing that it needs to attract the kind of members that brokers bring in, the California Exchange Board voted to pay brokers the same commissions in the exchange as they get for selling insurance out of the exchange. The Board also recognizes that exchange members can benefit from the kind of expertise that only health insurance agents and brokers can provide.
Group rates will rise so that the lower commission rate that brokers will receive from the carriers will be based on a higher premium. In addition, as employers look for creative solutions to rising healthcare costs, there will be more opportunities to sell voluntary benefits, such as critical illness, Medicare supplements, and accident plans. And when you sell more products, retention goes up, Crosby noted.
At press time, we are awaiting results of the presidential election. But, regardless of who occupies the White House, Nelson expects health reform provisions to continue to be watered down. “If Romney is elected, we will see faster watering down of the bill,” he said. However, he notes that the Obama Administration recognizes that the private sector has a role to play in health care delivery and has even invited the head of NAHU to the White House. In officially opening the SeeChange Health Broker Expo, Alan Katz, executive vice president of the company, noted that that healthcare reform will continue to exist regardless of the election because the status quo is not sustainable.
Selling Value-Based Benefits
Rod Grant, vice president of sales for SeeChange, explained how value based health plans fit into the new health care environment and how to present them to clients. Like traditional medical plans, value-based plans cover medical treatment and services when there’s an illness or accident. But, they also provide financial rewards when members take actions to improve their health. Rewards may include the following:
• Enhanced benefits with lower out-of-pocket expenses.
• Contributions to a health incentives account (HIA).
• Enhanced benefits and contributions to an HIA.
• A deductible credit.
Value-based benefits help member identify health problems earlier because they are motivated to be proactive about their health. And having an earlier diagnosis can make a big difference in a person’s quality of life while reducing overall medical costs.
Grant noted that health care reform is forcing every player in America’s health care system to justify their role. Too often, brokers are viewed only as sales people and not as problem solvers. By selling value-based benefit plans and wellness initiatives, brokers can address their clients’ total needs and help build a healthy and productive workforce, which boosts the bottom line.
Grant said that it’s also important to educate clients on the following positive aspects of the PPACA:
• Tax credits for offering group coverage (If applicable).
• Dependent coverage available for children up to age 26.
• Preventive health care mandates.
• The elimination of lifetime maximum limits
Who is a prospect for a value-based plan? Any current or potential client is a prospect. “There is no preferred industry. But our current top industries are medical, insurance, finance and law,” he said.
When offering a value-based plan, the first step is to gather information for a needs analysis:
• Have you had any rate increases in the past three years?
• What do you enjoy the most about you benefits?
• What is the most pressing concern your company has about the benefits you offer?
The next step is to gather information for a benefits assessment:
• What is your current healthcare insurance carrier?
• What type of coverage do you have – HMO, PPO?
• What are the deductible, co-insurance, and out-of-pocket maximums?
The next step is to compare rates and plan design. Seek out premium savings options. Start with a comparison of out-of-pocket maximums, co-insurance, and prescription drug exposure.
They key is to look for the best long-term value. Compare the current carrier’s average rate increases, for the past five years, to the plan you are suggesting. Also, compare the current carrier’s overall rate increases to the new carrier’s overall five-year performance.
Explore funding options for HSA or HRA plans; seek out a third-party HSA and HRA specialist; and calculate employer and employee savings opportunities. Define the options clearly if your client is considering replacing an HMO with an HSA or HRA.
The next step is communicating with your client:
• Give a detailed explanation of standard versus enhanced benefits.
• Stress that there is no additional premium cost with a value based plan.
• Mention that the employer can save by being proactive instead of just waiting to be hit with rate increases.
• Explain enhanced benefits that participating members enjoy.
• Advise the employer of tax credits, over age dependent coverage, preventive health care mandates, and the elimination of lifetime maximum limits.
• Conduct enrollment survey.
Legal Issues for Brokers and Their Clients
Brokers packed into a breakout session, “Laws Brokers Should Not Break” by Daniel Boivin, chief legal officer for SeeChange. (To get the full presentation, along with disclaimers saying that it’s not actually legal advice, download the presentation from www.seechangehealth.com/expo.)
Boivin illustrated how insurance agencies face the pitfalls of HIPPA and HITECH. In 2008, a rep’s laptop was stolen, which contained the personal information of local school district employees. The local press named the agency and reported that the laptop contained names, birth dates, Social Security numbers, and medical history information. The agency responded that the laptop was password protected, but did not make it clear whether the data was encrypted.
A complaint about an insurance agency was lodged on a website where people seek legal advice. According to the complaint, an agent called the wife’s workplace to follow up about her information on the medical history section of an application. She was not at the office, so instead of calling back, the agent asked her secretary to answer personal medical-related questions!
Boivin also detailed compliance issues with Medical loss rebates and summary of benefits and coverage. He stressed that, when it comes to these complicated laws, there will be compliance breaches, so it’s important to protect yourself from civil and even criminal liability. He suggests that employers do the following:
• Conduct annual training and keep signature logs.
• Require all new hires to complete training immediately.
• Do background checks of hires.
As the Expo wrapped up, it became clear that employers have many questions about how to respond to health reform and that it’s time to get busy working on the answers instead of worrying about the sky falling. q
––––––––––
Leila Morris is senior editor of California Broker Magazine
Exchanges Bring Big Opportunities for the Industry
The following is based on a comprehensive analysis by PWC Health.
by Leila Morris
The new state-based exchanges represent a major business opportunity for the insurance industry – an estimated $205 billion in premiums by 2021. One year from now, 12 million Americans are expected to begin purchasing health insurance through exchanges. Federal subsidies will entice many to the program with coverage starting in 2014. By 2021, the exchange market is expected to more than double, marking the largest expansion of health coverage since the creation of Medicare in 1965.
“This is the largest open enrollment in our careers,” said Kim Jacobs, vice president of product and innovation at UPMC Health Plan. Individual state exchange members in 2021 are projected to range from 100,000 in states such as Maine to 3.5 million in California. “Public exchanges will create an irreversible shift in the insurance market that will ultimately change the way medical care is sold in the U.S.,” said Joel Ario, managing director of Manatt Health Solutions and the former head of insurance exchange planning at HHS.
Private Exchanges
Private, employer-focused exchanges have much to gain. Unbounded by public exchange requirements, private exchanges can experiment with different approaches and adapt rapidly to consumer demands. They may lead the way in the quality of customer experience. “In an exchange, employees spend money differently than employers think. Individuals often buy up when they understand their choices,” said Ron Goldstein, president and CEO of CHOICE Administrators. Choices can include services such as vision, chiropractic service or more coverage for family members. “We’ve relied heavily on the broker network to educate the individuals; as more choice is introduced into the system, we’ll need the brokers to continue to play that educator role,” he added.
Ario said, “Private exchanges, already up and running in a handful of markets, may serve as innovation models in this new purchasing environment targeting employers and consumers seeking lower costs, greater transparency and convenience.” In many ways, the private exchange is the precursor to the public exchanges envisioned in the ACA. In the future, private exchanges will create an alternative for employers and for individuals who don’t qualify for government-subsidized insurance.
Private exchanges offer an alternative for employers to move toward a defined contribution approach that caps costs while offering access to a wider array of benefits. Starting in March 2013, employers will be required to notify employees about the new exchanges, providing detailed information on services offered and subsidy eligibility. The business must also clarify that it will not provide a contribution toward coverage if the employee enrolls in an exchange plan.
Medicaid Managed Care
Medicaid Managed Care organizations, which have experience addressing the needs of a lower income population, may be well-equipped to serve the market. In the latter years, the average income of exchange participants trends slightly upward as higher income people join the exchanges. For example, in 2014, HRI estimates that 16% of the individual exchange population will have incomes above 300% FPL. The portion rises to 35% in 2021.
Challenges for Insurers
For carriers, thriving in this new market won’t be easy. Insurers will need to maintain a balance of healthy and sick members to limit adverse selection. Providers and insurers will face challenges in serving a new customer base with a demographic profile and health needs that differ from today’s insured population.
Insurance companies must determine how to price at the different levels of plans laid out in the ACA – bronze, silver, gold and platinum – each having cost sharing percentages. Consumers care about price; with all else being equal, price will win. That’s where health plans will start competing in the exchanges. Some plans will price low to attract new customers while some may price higher to avoid the sickest, costliest patients. Higher-priced plans with a better fitting provider network could beat out some lower-priced plans. As previous HRI research has shown, 47% of consumers are willing to pay more for additional insurance features, such as dental or vision coverage. Even more important to consumers is the quality of insurance coverage. Consumers cited benefits and provider network as their top two aspects that define quality. Lower costs came in third.
Insurers focus on finding the sweet spot in product pricing and managing the influx of enrollees. It may be easier for larger insurers to turn a profit under the small margins, said Ario. Large-scale acquisitions are a likely outcome. However, regional insurers and accountable care organizations could provide tough competition to larger companies in markets with fewer players because they know their customer base and they can be competitive on price and benefits.
The pace of state exchange planning poses challenges for insurance companies. The timeline to begin qualifying health plans begins in October, but no state is ready. High progress states, such as California and New York, hope to begin health plan certification in early 2013. Only a few carriers may find it realistic or worthwhile to participate in all 50 public exchange markets.
Plans will compete head-to-head in the exchanges and against plans operating outside of the exchanges. Increased competition and pricing transparency will pressure insurers to control costs while maintaining benefits and quality. As the insurance exchange population becomes more demanding, plans will need more than price to attract and retain members.
Insurers that decide to compete in an exchange must keep a careful eye on administrative costs. Plans must already keep these costs below 15% to 20% of premiums under the ACA’s medical loss ratio requirements. Even if the company does well, it will be required to relinquish a portion of profits above 3% for the first few years as part of the “risk corridor function,” which is a temporary program that limits gains and losses by insurers operating in the exchange. And while there are controls in place to limit plan loss and liability from high-cost members, there are no guarantees of long-term profitability.
In addition to public exchanges, insurers look for opportunities in the private exchange world, including with small businesses. Insurers may work to create their own single carrier exchanges or participate in broader third-party exchange networks. As the environment shifts to a direct-to-consumer market, segmentation will be an important means to offer differentiated products to consumers and potentially also manage risk. Winners are likely to find a way to communicate with consumers in a way that non-healthcare professionals can understand.
Insurers will put pressure on providers to deliver value over volume. Enrollment in exchanges could speed up new expectations of care such as more online capabilities, improved transparency, and an increased focus on customer experience.
Provider Organizations
Once the exchanges are established, expect to see provider organizations developing products to compete with insurers on all lines of business. Provider-owned health plans and ACOs could be well positioned, said health industry investor Stephen Jackson. They will be able to offer lower-cost products with the advantage of local name recognition/reputation and insurers could become the backroom for these organizations.
Pharmacy Benefits
Depending on the type of benchmark plan selected by states, there will be various pharmacy benefit structures ranging from restrictive formularies to a comprehensive benefit similar to that offered through the Federal Employee Health Benefits Program (FEHBP). Over time, qualified health plan participation rules may impose additional requirements, such as evidence that demonstrates superiority to medications and devices already covered in a therapeutic category. If more states choose to adopt the FEHBP open formulary design as a default, it could be a boon for branded drug manufacturers looking for continuity and maximum pharmaceutical coverage. On the other hand, more limited formularies would further drive usage of generic medications. Generous purchasing subsidies built into the ACA provide a large and rapid cash injection into the burgeoning health insurance exchange market.
Employers
Many employers will not see dropping their health benefits as a viable solution. The ACA’s $2,000 penalty for dropping coverage for a full-time employee may seem small compared to the cost of providing health insurance. But that penalty multiplies. The annual penalty calculation is the number of full-time employees minus 30, times $2,000. The penalty grows each year by the growth in insurance premiums.
Employers that drop coverage lose numerous tax advantages that come with offering health benefits. Also, employees view healthcare as a valuable benefit. The employers that are most likely to consider dropping coverage are those with high concentrations of lower-wage workers who will qualify for federal subsidies through the individual exchange markets.
With the law and its subsidies, exchanges could revolutionize the health insurance market by shifting the focus to the individual and prompting insurers to act in a more retail-oriented manner. There will be a push for clarity in products and their value, convenience for buyers and competitive prices. Yet the 2010 law is neither the first nor the last word on the future of exchanges. Even if a future Congress and administration scale back or repeal the law, exchanges remain a hot prospect, as evidenced by the private sector entering this new market.
Investors view 2014 as the start of a major new trend in the US health system – away from employers managing coverage to a robust, open marketplace. Ongoing cost concerns will continue to spur change, both in the form of commercial innovation and more traditional government pressure. Under the ACA, regulators already have MLR limits on premiums and the power to review rate increases. In addition, states may follow Massachusetts in implementing all-payer pricing systems for providers.
The Congressional Budget Office projects that exchange membership will reach 25 million in 2021 for the individual exchange and 4 million for the small group exchange.
Exchange shoppers are not likely to overwhelm the healthcare system or substantially drive up costs immediately after gaining coverage. However, they will be less familiar with the insurance system; in 2014, approximately 75% of public exchange enrollees will be newly insured. Over time, outreach and education efforts by states and insurers will need to match the changing needs of exchange members as they transition from newly-insured to more sophisticated customers. To get the report, visit http://pwchealth.com/cgi-local/hregister.cgi/reg/pwc-health-insurance-exchanges-impact-and-options.pdf.
Dental–Diabetes Month Brings a Renewed Focus on Periodontal Disease
by Dr. James Bramson
During American Diabetes Month in November, it is important for you and your clients to know that periodontal treatment and ongoing maintenance can decrease the annual cost of medical care for people with diabetes.
Earlier this year, United Concordia Dental conducted a landmark study with parent company Highmark and the University of Pennsylvania. It showed that a significant reduction in hospitalizations (33%), physician visits (13%) and overall medical costs ($1,184 per year) is possible when individuals with diabetes receive treatment for gum disease. This study is the largest of its kind showing a connection between oral health in diabetics and medical costs conducted by renowned researcher and former dean of the School of Dental Medicine at the University of Pennslvania, Marjorie Jeffcoat.
The study analyzed data over a three-year period from nearly 1.7 million individuals with both Highmark medical coverage and United Concordia dental coverage to determine the effects of proper periodontal care. When you look at the study’s sheer size and scope, as well as its statistical significance, it is clear the results are no fluke – when diabetics have their periodontal disease treated, it not only helps them become healthier, but it also helps them and their employers save money in the long run.
Today, there are 25.8 million individuals with diabetes in the United States – double the amount in 1999, according to the Centers for Disease Control and Prevention. And that number continues to grow at a startling pace.
This study underscores the need for a commitment to wellness by dental insurers, dentists, employers, and producers. It also demonstrates a good practice for the dental industry to embrace. Treating chronic health conditions is a very high cost; dental disease is preventable at a much lower cost and the beneficial effects through reduced medical costs can be significant. These findings related to diabetes represent the first in a series of conclusions suggesting how appropriate dental treatment and maintenance can help predict lower medical expenses for various chronic medical conditions.
Over the coming months, researchers will examine the pharmacy benefits cost impact of treating periodontal disease in diabetics, followed by individuals treated for this disease who experienced pre-term births, heart disease and stroke. If the results of this study can be mirrored with other diseases, some significant health savings should be shows there, as well. This would broaden the argument for why it makes sense to treat someone’s periodontal disease across a variety of different conditions.
––––––––
Dr. James Bramson is chief dental officer at United Concordia, where he directs the professional relations department, professional quality assurance activities, utilization review, claims review process and clinical aspects of product offerings and communications. Dr. Bramson has 30 years of dental industry experience, including national experience as executive director of the American Dental Association (ADA) and secretary of the ADA Foundation.
Dental–A Good Dental Wellness Program In Your Portfolio Could Mean Increased Sales
by Timothy Custer, D.D.S.
For many people, the concept of dental wellness begins with a parental command to brush regularly and continues into adulthood with a semi-annual or less frequent directive from a dental hygienist to floss more thoroughly and more often. But my colleagues and I believe that dental wellness involves more than just two checkups each year. We believe the following:
• Dental wellness is strongly linked to overall wellness.
• A well-designed and well-implemented dental wellness program can improve overall health in an employee group.
• The broker who can offer and explain a proactive dental wellness program will have a competitive advantage in seeking group health business.
Dental Problems Don’t Stop In The Mouth
When we think of dental problems, fillings, extractions, and root canals spring to mind. True, those are common and often costly. But, periodontal disease looms larger in prevalence and far-reaching detrimental effects than any of those. Periodontal disease, a chronic inflammation that affects gums and/or the bone that supports the teeth, is found in 47.2% of Americans 30 or older, according to the Centers for Disease Control, in a study published in the Journal of Dental Research. Even more alarming, that percentage rises to 70.1 for those 65 or older. According to the co-author of the Journal of Dental Research study, “We now know that periodontal disease is one of the most prevalent non-communicable chronic diseases in our population.”
Clearly, periodontal disease leads directly to increased claim costs in a dental insurance program in the form of treatment for the disease itself and for the tooth loss that can easily result from it. But that’s the least of the problems it can cause.
A study in the Journal of Periodontology reveals a two-way relationship between periodontal disease and diabetes. On the one hand, periodontal disease can contribute to diabetic complications, such as increased blood sugar. On the other hand, a poorly controlled diabetic is more likely to develop periodontal disease. Studies have also explored links between periodontal disease and such conditions as chronic kidney disease, rheumatoid arthritis, chronic obstructive pulmonary disease, cardiovascular disease, and stroke. (A number of media releases at www.period.org/consumer/media/releases.htm, reference studies suggesting a connection between periodontal disease and other medical conditions.)
Dental Wellness Programs Can And Do Help
Some dental programs promote dental health, but they limit services or benefits. They may shift more of the costs to the insured in the form of increased co-pays and deductibles or lowered maximum benefits. These approaches can demonstrate short-term savings for the employer, but we do not believe they show long-term benefits.
More effective dental programs take a proactive approach, offering a balance of effective treatment, financial incentives, and wellness education. We believe these programs will have more cost-saving effects in the long-term.
For a start, from the data they already have, carriers can identify portions of the population at risk for dental disease and target them for messages and reminders. These demographic cohorts would include employees with diabetes or cardiovascular complications, and those who simply have not been to a dentist for a cleaning in more than a year.
Surprisingly, a high-risk group that’s often overlooked is the very young. Mothers can easily spread the kind of bacteria that cause cavities to their newborns and parents may not automatically think of scheduling dental appointments until their children are a few years of age if problems have not already manifested themselves. By then, it may be too late to head off conditions that could have easily been nipped in the bud with earlier treatment.
Once the high-risk groups have been identified, targeted mailings can be directed to them. It would be tempting to say that such reminders won’t do much good if the admonitions of our parents and dentists haven’t spurred us to better oral hygiene, but our experience proves the opposite. In the past two years, we mailed more than 400,000 educational flyers to a variety of members in various high-risk categories. Those receiving the mailing included dental plan members who had not visited the dentist in the past year. Remarkably, in certain risk populations nearly 40% of members who had not seen a dentist in the past 12 months did so after getting the educational mailer.
Of course, these days, no educational communication and outreach program can be considered complete without an online component. Increasingly, people are as receptive, if not more so, to online materials as they are to mailings or face-to-face contact. Those who don’t read an article they receive in a directed mailing may happily read the same material from a database of informational material. And those who would prefer not to talk to a dentist in person might happily seize the opportunity for the relative anonymity of a website’s ask-a-dentist feature.
Dental Wellness Programs As A Competitive Advantage
Before you can make a dental wellness program work to your benefit, three steps are necessary. First, you have to believe in it yourself. I hope that this very brief article is the beginning of that belief, and I urge you to check the wealth of material associated with dental health and overall health that is available at the American Academy of Periodontology website, www.perio.org.
Second, you have to find a carrier that offers a proactive dental wellness program. When you talk to your carrier’s representatives, ask what they’re offering and make sure to get more details than simply, “Yes, we have one of those.”
Third, you have to convince your clients that a dental wellness program will pay off for them in terms of overall employee satisfaction and health, not to mention the decreased absenteeism and claim costs. Some of your clients will be convinced that they have enough different programs in place and will resist adding yet another. It’s your job, with the help of your carrier, to convince them that the link between dental health and overall health is real and demonstrable, and a complete wellness program should include dental wellness as well.
–––––––––
Timothy Custer, D.D.S. is dental director for Dearborn National.
Dental–A Case for Selling Dental Insurance to Small Companies
by Tom Morey
More than one-third of Americans don’t have dental insurance, according to a recent report by the U.S. Senate Committee on Health, Education, Labor & Pensions. The demand from today’s workers is being heard loud and clear. Dental is the third most demanded benefit after major medical insurance and retirement benefits. So why aren’t some smaller employers offering it?
What Employers Have to Lose
Small businesses success is related directly to having employees who are productive, present, and focused. That’s why workers’ personal problems and health concerns can have such a detrimental effect on business operations. Small companies identified “increasing employee productivity” as their top goal, according to the 2012 Aflac Workforces Report, conducted by Research Now.
Health and personal issues seem to greatly diminish productivity at our nation’s small businesses. Thirty-eight percent of employers say that health problems contribute to their employees’ greatest work distractions. On average, employers say that 22.1% of work productivity is lost due to personal issues. That equates to approximately 168 hours per week in lost productivity.
Employed adults lose more than 164 million hours of work each year due to oral health problems or dental visits, according to a fact sheet by the Centers for Disease Control and Prevention.
Small business employers have expressed the best intentions to establish benefit programs that take care of employees, yet nearly half of workers at small companies say their benefit packages do not meet their needs or their families’ needs. Employers may not realize that protecting intellectual capital also protects their financial assets and that offering a benefit package that best meets employee needs helps attract and retain talented employees.
Almost half of American workers say they are likely to look for a new job in the next 12 months, according to the Aflac study. Additionally, half of employees said “Improving my benefit package is the one thing my employer could do to keep me in my current job.” Sixty-one percent said they are likely to accept a job offer that comes with lower pay, but better benefits. This goes to show how seriously employees value their families’ health and well being.
A Voluntary Dental Solution
Trends in the dental insurance industry create an opportunity for competitive voluntary dental insurance policies. Approximately 32% of small businesses would offer dental insurance to employees if they could afford the premiums, according to a LIMRA survey. That makes voluntary dental insurance, which is at no direct cost to employers, a smart choice for small businesses.
Some voluntary dental insurance policies differ from traditional dental insurance in that they have networks, deductibles, or precertification requirements and no annual premium reviews.
No Networks
A voluntary insurance policy isn’t tied to a provider network unlike a dental HMO, PPO or other type of dental plan. Employees enjoy the freedom and flexibility of going to any dentist. Also, it eases the burden on employers and brokers to evaluate or negotiate networks with the insurance provider.
Easy Administration
Business owners want simple and hassle-free benefit solutions. Paperwork is greatly reduced by rapid claims processing and no annual premium reviews. This reduces the time spent on renegotiating and administering the dental plan.
No Deductibles
Many dental plans require deductibles to be met each year. “No deductibles” spells “sign me up” for many HR decision-makers. With the right provider, routine or emergency claims are processed quickly and easily on a voluntary plan without the financial burden of a deductible for any qualifying treatment.
No Pre-certification Requirements
Americans are juggling multiple personal, professional and household responsibilities. And getting dental work is already a highly undesirable task for many people. Who wants to spend extra time getting approval or referrals for permission to see certain dentists or specialists? Voluntary insurance skips the red tape and puts employees at the front of the line for care.
No Annual Premium Reviews
Policy rates do not increase based on utilization or group demographics. When an employee pays for their voluntary plan in whole, it usually means that the employee has complete ownership of their plan. That’s a major value-add for employers since they can focus on running their business instead of regularly reviewing or renegotiating the dental plan on the employees’ behalf.
In addition to these valuable benefits, voluntary policies can be portable and are guaranteed-renewable for as long as the premiums are paid.
For the majority of small companies, the second largest benefit challenge is offering robust benefits while staying within budget. As brokers find solutions for employers and benefit decision-makers, dental insurance can actually be one of the easiest pieces of the benefit puzzle to complete. Because voluntary dental insurance does not require employers to make a premium contribution, 15% of employers that offer dental coverage are likely to move to voluntary coverage in which employees pay 100% of the premium, according to a study by the National Assn. of Dental Plans.
Moreover, 60% of employees say they would be likely to purchase voluntary insurance benefits if their employer offered these benefits, according to the Aflac study. This shift to voluntary dental plans opens a wide door for insurance brokers, creating a potential voluntary sales opportunity of $225 million, approximately 11% of the $2 billion dental insurance industry, according to a study by Eastbridge Consulting Group. Small business decision-makers must deliver more effective benefit packages in order to help employees protect the well-being of themselves and their families. By doing so, they’ll protect their companies against declining productivity while retaining their all-important intellectual capital.
–––––––––
Tom Morey is Vice President of Product Development at Aflac.
Our Annual HMO Survey – Pt. II
Retrieving Information on HMOs
Our Dogged Research Pays Off
Welcome to the 16th annual agents’ guide to managed care. Each year California Broker surveys health maintenance organizations (HMOs) in the state with direct questions about their plans. We then present the answers to such questions here for you – the professional agent or broker. We hope that this valuable information will help you serve your savvy healthcare clients better.
22. Is your plan NCQA accredited?
Aetna: Yes, Aetna Health of CA Inc is accredited and has gotten a Quality Plus distinction in Care Management, Physician and Hospital Quality.
Anthem Blue Cross: Anthem Blue Cross and Anthem Blue Cross Life and Health Insurance Company have achieved a Commendable Accreditation rating from NCQA. NCQA awards a status of Commendable to organizations with well-established programs for service and clinical quality that meet rigorous requirements for consumer protection and quality improvement.
Cigna: Yes, our HMO plan has received NCQA’s highest accreditation level of “Excellent.” In addition, Cigna has earned NCQA’s Physician and Hospital Quality (PHQ) Certification. These standards assess how well a plan provides individuals with information about physicians and hospitals in its network to help them make informed health care decisions. Cigna has also earned an NCQA quality rating for its health and wellness programs, and all four of our behavioral health care centers nationwide have earned full accreditation from NCQA.
Health Net of CA: Yes, commercial HMO, PPO, and POS lines of business have received the Commendable accreditation status from the National Committee for Quality Assurance (NCQA), and Health Net’s Medicare HMO received the Excellent accreditation status.
Kaiser Permanente: Yes, we are. As of the third quarter of 2012, all of our service areas across the country have NCQA ratings of Excellent for our HMO and Medicare lines, which is their highest possible rating.
PacifiCare: Yes, PacifiCare of California maintains an excellent accreditation rating.
23. What is your ratio of PCPs vs. specialists?
Anthem Blue Cross: 1:2
Cigna: Data not available
Health Net of CA: 2012: 1 to 3.0 specialists.
Kaiser Permanente: The statewide ratio in California of primary care physicians to specialists is approximately 1 PCP to 1.8 Specialists. Primary Care includes General Practice, Family Medicine, general Internal Medicine, and general Pediatrics. Specialty care includes OB/Gyn.
PacifiCare: As of June 30, 2011, our ratio of PCPs to specialists is 1 to 3.1.
24. What is your ratio of members to PCPs?
Aetna: 21:3
Cigna: 14/1
Health Net of CA: 2012: 66.0 members to 1 PCP.
Kaiser Permanente: We don’t ordinarily release information on our member-to-doctor ratio. Physician and care provider totals are based on current and projected membership numbers. Providing members with access to physicians is essential to delivering high-quality care, and to ensure it, we have developed access standards to help meet our members’ needs. Monitored continuously, these standards are used to help determine the number of physicians and care providers needed as well as the location and size of our medical facilities. As dictated by membership growth and increased volume of patient visits, additional primary care physicians and specialists are added to our professional roster as needed.
PacifiCare: As of June 30, 2011, our ratio of members to PCPs is 131 to 1.
25. Does your contract include binding arbitration?
Aetna: Yes.
Anthem Blue Cross: Yes, our HMO contracts include binding arbitration language.
Cigna: Yes.
Health Net of CA: Yes.
Kaiser Permanente: Yes, we use binding arbitration to resolve disputes. We find arbitration to be more attuned to the discussion of sensitive matters such as medical and more appropriate for the resolution of disputes with persons who, in many cases, continue to be Health Plan members. Other than Small Claims Court cases, claims subject to a Medicare appeal procedure, or ERISA-regulated benefit claims, arbitration is used to resolve disputes such as those for premises or professional liability matters, including claims alleging medical malpractice.
PacifiCare: Yes, our contract includes binding arbitration.
26. How often can members change their PCP at will?
Aetna: There is no limit.
Anthem Blue Cross: Our HMO member may change to another PCP without restriction. Members may change to a PCP at another PMG/IPA by completing a membership change form and submitting it to their employer, or by calling customer service directly. Because we are concerned with continuity of care, members cannot switch medical groups during a “course of treatment;” however, based on individual need, changes to a PMG assignment can be made effective the first day of the following month after the request is made. Please note: members may only change to a medical group that is within 30 miles of their residence or work address.
Cigna: We encourage our customers to stay with one primary care physician to ensure more effective care management. We also recommend that people not change their doctor while in the middle of care to the extent possible. Customers may request a PCP change once per quarter and/or if their residence or work location changes. Additionally, if a customer has a concern about care quality, he or she can change PCPs after notifying us of the concern.
Health Net of CA: Members may change PCPs within a physician group or from one physician group to another once per month.
Kaiser Permanente: Members can change their PCP at any time and as often as they like. Members can change their PCP online at kp.org, by calling the Physician Selection Service or Appointment/Advice line at their local medical facility, or through the Member Services Department at their local medical facility. Studies have shown that a positive, ongoing relationship with their PCP helps to improve health outcomes and member satisfaction, so we encourage members to choose a PCP who’s right for them and provide the support and systems to make it easy for them to do so.
PacifiCare: Members may request a change of individual provider or provider group at any time, for any reason. Requests received between the first and the 15th of a month take effect on the first day of the next month. Requests received between the 16th and the end of the month take effect on the first day of the second month. Members must select participating providers accepting new patients within 30 miles of their home or work and can identify which providers are accepting new patients by calling our Customer Service department, looking in our provider directory or visiting our Web site.
27. Do you offer a performance guaranty, such as employees will be on the computer by a certain date or have ID cards by a certain date, for example?
Aetna: Yes, we can offer standard performance guarantees to our clients; guarantees may also be customized on a case-by-case basis.
Anthem Blue Cross: Yes, we can offer standard performance guarantees to our clients; guarantees may also be customized on a case-by-case basis, based on client size thresholds.
Cigna: Yes, in most instances, we can work with a company to develop appropriate performance guarantees.
Health Net of CA: Yes, Health Net of California negotiates performance guarantees with clients based on our Corporate Performance Standards, which are derived from marketplace expectations balanced with internal administrative capabilities. An employer group must have and maintain after the plan’s effective date a minimum of 1,000 subscribers in a Health Net of California plan to qualify for performance guarantee consideration. Once the client has been deemed eligible for performance guarantee consideration, Health Net is willing to discuss and negotiate the specifics of a performance guarantee package including appropriate target levels for standards of concern.
Health Net of California provides customers with specific performance guarantees in the area of claims administration, including processing turnaround time (measured within 30 calendar days) and transactional accuracy (i.e. financial, payment, coding and overall). In addition to claims administration, Health Net of California offers corporate performance standards that span all aspects of our business in the areas of: implementation (i.e., identification card production, timeliness and accuracy), member services, provider network, medical management, member satisfaction, customer reporting, and HEDIS reporting. All products can potentially be covered, with the exception of our Medicare HMO due to strict guidelines already in place by the Centers for Medicare & Medicaid Services (CMS). All performance standards are evaluated on an annual basis for compliance. An annual performance standard report, including the calculation of any applicable penalties, is produced approximately 90 days after the close of the plan year.
Kaiser Permanente: Yes, our performance guarantees are made on a group-by-group basis. Our target is for new members to be in our data base within 24 hours of our receiving their information and to have new or replacement ID cards delivered within 7 to 10 work days 90 percent of the time.
PacifiCare: We may agree to performance guarantees upon approval and if the client meets our standard requirements for enterprise-wide performance standards. However, we typically do not agree to performance guarantees for fully insured groups.
28. When a member moves out of state, is any transition coverage available?
Aetna: We have HMO plans in many states; a member might be eligible for coverage in another Aetna HMO service area. Customers may also offer out-of-area plans which provide PPO coverage if members are outside an HMO service area.
Anthem Blue Cross: The utilization management process is delegated to the PMGs/IPAs for our HMO product. They must have established review mechanisms, such as evidenced-based decision criteria and guidelines, which align with accepted medical practice. PMGs/IPAs maintain structured processes for referral management, pre-service, concurrent, and post-service review. Routine and active oversight is conducted to ensure compliance with regulatory and accrediting agency standards.
Cigna: Yes, if we offer similar coverage to the account in that state.
Health Net of CA: Yes, through PPO, POS, and indemnity lines of business.
PacifiCare: If a member moves out of the state permanently, they are no longer in our service area and would be terminated from the plan. Members must live within our service area to be eligible for continued enrollment in our health plan. Members traveling outside their PacifiCare service area for a limited time are covered for emergency services. This also applies to out-of-area student dependents who must also maintain a permanent residence within the service area in order to enroll in the health the plan.
29. Describe the utilization process.
Aetna: Information is gathered from the physician and patient. The nurse consultant or physician reviewer and the attending physician discuss whether a test or treatment is appropriate. The physician reviewer can recommend alternative treatments and further testing. Protocol is reviewed annually. The consulting specialists, who are most familiar with procedure, review and approve any changes.
Anthem Blue Cross: The utilization management process is delegated to the PMGs/IPAs for our HMO product. They must have established review mechanisms, such as evidenced-based decision criteria and guidelines, which align with accepted medical practice. PMGs/IPAs maintain processes for referral management, pre-service, concurrent, and post-service review. Routine and active oversight is conducted to ensure compliance with regulatory and accrediting agency standards.
Cigna: Cigna physicians and nurses perform utilization management for inpatients in coordination with medical groups. To help ensure appropriate care and facilitate discharge planning, Cigna reviews medical records for hospitalized customers and consults with physicians via nurses located on-site at hospitals or by phone. Utilization review for most outpatient services is delegated to IPAs/Medical Groups. Cigna reviews inpatient procedures and hospitalizations, outpatient surgical procedures performed in a facility, transplants, and investigational therapies using Milliman Care Guidelines and Cigna Coverage Positions. Cigna utilization nurses (RNs) also conduct case management. Most outpatient referrals for specialists and procedures do not require prior authorization as long as the primary care physician requests them. However, Cigna performs utilization review of select outpatient services when there is demonstrated value.
Health Net of CA: Health Net provides a multi-dimensional utilization/case management (UM/CM) program to direct and monitor health care services. It involves pre-service, concurrent, and post-service evaluation of the utilization of services provided to members. The UM/CM program is structured to ensure that qualified health professionals make medical decisions using written criteria based on sound clinical evidence without undue influence of Health Net management or concerns for the plan’s fiscal performance.
Kaiser Permanente: Our physicians plan member care and work collaboratively with their peers to ensure appropriate treatment plans and use of resources. Utilization Management staff are available to support doctors in the management of member’s health care needs throughout our continuum of care and provide a variety of services such as discharge planning, utilization review, and care management.
The majority of utilization management, including reviews, is conducted internally as part of our integrated system of health care delivery. Kaiser Foundation Health Plan, Inc., Kaiser Foundation Hospitals, and the Permanente Medical Groups work in partnership to provide and coordinate medical management and review for our Health Plan members.
PacifiCare: We use industry-leading medical management programs to ensure that each enrollee receives the appropriate care necessary and that we control unnecessary health care costs for our clients. Our medical management programs focus on reducing variation, improving the quality of care provided and ensuring cost effectiveness. We base medical decisions on scientific evidence and all of our medical management services include physician guidance and input. We developed online, science-based and objective utilization management criteria as well as technology-based clinical decision support systems related to case, utilization and disease management.
30. Describe the Case Management Process.
Aetna: The following are some ways in which cases are identified: through the PCP or pharmacy, during certification reviews, during PMG/utilization management case reviews, and through other internal reporting and sources including member services, claims, and specialty programs. The case manager coordinates services for members who have multiple and complex needs. The case manager works with the PCP and the member to develop a care plan identifying services, frequency, duration, and goals. A team approach includes the PCP, specialist, member, family, caregiver, healthcare provider community, and internal programs to coordinate care, with a focus on member education and maximizing quality outcomes.
Anthem Blue Cross: The PMGs/IPAs perform in-area case management functions. Anthem case managers support PMGs/IPAs for members with exceptional needs or complex medical conditions. When appropriate, they manage out-of-area emergency admissions and help with transfers to in-area care. They also facilitate communication between healthcare providers and ensure that appropriate follow-up care is arranged with the PMG/IPA.
Cigna: Customers are identified via real-time and claims-based predictive modeling tools, along with referrals from physicians and medical groups, Cigna clinical staff, and employers. Case managers collaborate with physicians, medical group case managers, customers, and employers to facilitate ongoing treatment plans and support the primary care physician. Case managers monitor short-term and long-term goals for inpatient and outpatient care. They document and evaluate the effectiveness of the services provided. In addition to traditional complex and catastrophic case management, Cigna has a number of specialty case management units. They are staffed with RNs who are dedicated to areas such as high-risk maternity, neonatal intensive care, oncology, obesity, and transplant. Cigna has an extensive suite of chronic condition management programs, including those for obesity complications and depression. Cigna also offers telephonic and online access to wellness information, care management services, and health coaching programs.
Health Net of CA: Health Net and its delegates provide case management/disease management programs to deliver individualized assistance to members in all lines of business who are experiencing complex, acute, or catastrophic illnesses or have exceptional needs. Health Net’s approach to utilization management extends far beyond traditional oversight. Health Net provides outreach to members with chronic conditions such as asthma, diabetes, COPD, heart failure, coronary heart disease, preference-sensitive conditions, and identification of members with cardio-metabolic risk; Health Net also uses population-based risk stratification and predictive modeling; and partners with physician groups to improve performance.
Kaiser Permanente: Members in need of case management are identified through clinical and utilization data, pharmacy records, hospital and outpatient visits, and laboratory results. Members can also self-refer to case management or be referred by a doctor or family member. Our case managers are master’s-level clinicians or registered nurses who work directly with a member and their health care team to plan care and provide intensive coordination of services, including inpatient hospitalizations, transitional care, home care, skilled nursing, medications, referrals to community resources, and outpatient care. Using an interdisciplinary approach, case managers help to ensure continuity of care including utilization management, transfer coordination, discharge planning, and obtaining all authorizations or approvals as needed for outside services for members and their families. They’re also responsible for identifying quality-of-care problems and monitoring utilization issues.
PacifiCare: We designed our case management program to identify, intervene, coordinate and monitor care plans that provide high quality and cost-effective care for covered persons with catastrophic and complex health care needs. Our case managers facilitate communication and coordination of care between all parties on the health care team. This program involves the patient and family in the decision making process to minimize fragmentation in the delivery of health care. The case manager assesses the needs of the patient and educates them and the health care delivery team about case management, community resources, insurance benefits, cost factors and issues in all related topics so that informed decisions can be made. The case manager is the link between the patient, the providers, the payer and community.
31. Can the PCP participate in profits or losses in any way at the plan level or the participating medical group/IPA level?
Aetna: In California, Aetna participates in the IHA/7 health plan program of pay-for-performance. PCPs can participate in that IPA pay-for-performance bonus.
Anthem Blue Cross: Anthem established one of the first pay for performance programs in California. We encourage our PMGs and IPAs to maintain a physician rating system with appropriate rewards for quality medical care. Physicians will get increased compensation for quality care. Our contract is not with the individual PCP. It is with the PMG/IPA with which we have risk sharing arrangements. Through a risk sharing arrangement we share cost savings for in-patient, emergency room, outpatient services and generic prescription rates with the PMG/IPA. The medical group/IPA may get incentives up to 50% of savings depending on the amount of costs saved.
Cigna: The primary care physician does not participate in plan profits or losses in any way. The relationship between the PMG/IPA and the PCP is based on the contract between the two parties.
Health Net of CA: In 1993, Health Net of California introduced the Quality Care Improvement Program (QCIP). At the time, it based medical group compensation on member satisfaction scores. This program was enhanced in 1998 by incorporating quality-of-care outcomes into the compensation formula. In addition to contracted compensation, QCIP evaluates medical groups based on member satisfaction rates, quality-of-care outcomes, and collaboration. Additionally, Health Net evaluates medical groups’ cost performance measures. Similar to most health plans, shared-risk pools are incorporated with the compensation details for each Participating Physician Group (PPG). When the budget is established for the PPG’s medical services and hospital care, the PPG shares in the savings if costs do not consume the budget. Conversely, the group shares in paying for additional costs if the cost of care exceeds the budgeted amount. However, at no time does Health Net favor cost performance over quality. Recently, other California health plans have added programs similar to Health Net’s QCIP.
Kaiser Permanente: All of our physicians are eligible for incentive payments based on their own performance as measured by the results of member satisfaction surveys, the quality of care provided to members as perceived by their peers, administrative goals such as their adoption of techniques to allow them to provide better care, and by the overall performance of our organization. Incentive payments make up a very small part of our physician’s annual renumeration.
PacifiCare: We use a Quality Incentive Program (QIP) through which medical groups and IPAs can earn additional revenue by improving and maintaining patient safety, patient satisfaction, and quality of care. The QIP measures key indicators of quality in hospitals and medical groups based on the groups’ service and clinical quality. The QIP rewards medical groups and IPAs for attaining the required performance. The better a provider group performs in these categories the more QIP dollars they can earn. In 2003 the QIP was funded with $14 million and rewarded seventy-fifth percentile performers in 16 measures. Over 140 medical groups received rewards in 2003 and we achieved average mean score improvements in 12 of the 16 measures. In turn, average improvement for these measures increased 30 percent, a remarkable achievement. In 2004 our QIP expanded to include 20 measures, of which 17 improved an average of 20 percent. The incentive pool was $18 million in 2004 and is $65 million in 2005. In 2006, we paid out more than $96 million.
32. How are premiums and risk shared among the plan, MG/IPA
Aetna: The premium is not shared with providers. In California, we have some IPA risk share arrangements and an IPA or medical group share in savings if a target budget is not exceeded.
Anthem Blue Cross: Anthem has a capitated arrangement with the PMG/IPAs, which are responsible for payment of professional services. We promote clinical efficiency through a program of shared savings between the PMG/IPA and Anthem for expenditures related to capitated professional services. We have a program to share the savings for non-capitated inpatient care, outpatient care, and generic pharmacy prescription. Anthem is the largest sponsor of the IHA performance measures in the state and has the second largest pay for performance program in world behind only the United Kingdom’s.
Cigna: Most medical group and IPA arrangements are capitated. Capitation does not contain provisions for withhold payments. For example, a lump sum is withheld and distributed later if the provider meets certain utilization targets. The standard contract is shared risk with Cigna retaining risk for inpatient facility charges.
Health Net of CA: The majority of HMO physician services are paid under a pre-paid capitation payment to the contracted participating physician group (PPG). The PPG, in turn, reimburses the physician directly for services.
Kaiser Permanente: Kaiser Foundation Health Plan (KFHP) contracts with the Permanente Medical Group (TPMG) in Northern California, and the Southern California Permanente Medical Group (SCPMG) to provide comprehensive medical services to KFHP members. The contractual arrangements are reimbursed at negotiated capitation rates as set forth in itemized budgets. The medical groups are reimbursed at negotiated capitation rates. A small portion is paid on an actual cost basis for specific items. Subject to limits on risk sharing, the medical groups are fully at risk for the capitated portion. They share the risk equally with the health plan for the actual cost portion.
PacifiCare: Currently all of our contracted medical groups and independent physician associations (IPA) participate in a risk-sharing arrangement. In addition, we contract with several networks of individual physicians in rural areas that do not participate in risk sharing. We contract with multi-specialty medical groups and independent physician associations (IPA) primarily through split or professional capitation contracts. Both contracts provide a monthly age, gender and benefit adjusted capitation.
33. What happens when a member provider bills a participant for services? How do you deal with the fact that the participant is at financial or credit risk when the dispute is between the provider and the plan?
Aetna: Participating providers are required to accept payment (plus member’s co-payment) as payment in full. Balance billing is not permitted.
Anthem Blue Cross: Our first priority is to protect our membership from inappropriate billing. Our HMO providers are contractually required to refrain from billing members except for co-payments. If a participating provider bills a member, it is brought to the attention of the PMG/IPA liaison and the PMG is directed to pay the claim. If the PMG does not pay the authorized claim in 45 days from receipt, the plan pays the bill and debits the PMGs capitation payment for the ensuing period.
Cigna: First, it’s important for customers to know that using hospitals and doctors who are a part of the network protects them from balance billing because in-network health care professionals agree as part of their contracts not to bill individuals for amounts beyond what their plan pays. If Cigna receives a complaint from a customer who has received such a bill, we work with the contracted health care professional to educate him/her on the terms of the contract. We also require that the health care professional stop billing the customer. Our customer service representatives are available by phone 24 hours a day, seven days a week to assist our customers with any questions about a claim or bill they have received. We also work with our health care professional partners to make the claim payment process as efficient and accurate as possible.
Health Net of CA: Health Net’s HMO contracts have a hold-harmless clause that prohibits medical groups from billing or collecting from members, except for standard co-payments and non-covered services. In the event a provider balance bills a member, Health Net removes the member from the situation and resolves the matter directly with the provider.
Kaiser Permanente: As a precipitated group practice HMO, we do not bill members for individual services. Kaiser Foundation Health Plan (KFHP) contracts with The Permanente Medical Group (TPMG) in Northern California and the Southern California Permanente Medical Group (SCPMG) to provide comprehensive medical services exclusively to KFHP members. Our providers are reimbursed at negotiated capitation rates so no disputes between the providers and the health plan would put members at financial or credit risk.
34. Do you have a nurse or RN on call 24 hours for questions at the plan level? At the PMG/IPA level?
Aetna: Yes, the Informed Health nurse-line is available to members. Network doctors are required to be available 24 hours a day.
Anthem Blue Cross: Anthem has a 24/7 Nurse Advice Line that is available for members. The member’s PCP or other covering practitioner is available to the member after hours and on the weekends if needed for non- emergent issues. The member may access the emergency room as needed for emergencies.
Cigna: Yes, CIGNA offers a 24-hour health information line staffed with nurses.
Health Net of CA: Health Net’s Nurse 24 line offers support for both members and physicians. Members can obtain support on a 24/7 basis from experienced clinicians. The clinicians are nurses licensed in the member’s state and are ready to provide support for members for health and wellness concerns, decisions, and questions. Physicians can make referrals on a 24/7 basis via Health Net’s provider portal. Physicians can also receive support, make referrals, and get information during business hours by calling 800-893-5597 and pressing option #2.
Kaiser Permanente: Yes. Members can easily reach our specially trained advice nurses by telephone 24 hours a day, seven days a week. Using approved protocols, our advice nurses perform comprehensive triage to help members assess their symptoms and determine the level of care they need, such as self-care, an appointment with their PCP, a visit to urgent care or emergency department, or a call to 911. When certain criteria are met, our advice nurses can also arrange for “telephone treatment” where members can get needed prescriptions for certain common conditions-including urinary tract infections, conjunctivitis, and sinusitis-without having to make an unnecessary visit to urgent care or their doctor’s office. Our nurse advice service is fully integrated into our system of care, not a separate carved-out service. This integration gives our advice nurses instant access to information in our members’ electronic medical records, which enables them to provide more individualized assistance to our members. It also makes it easy for an advice nurse to send a message to the member’s personal physician about the call and its outcome and, when appropriate, facilitate continuity of care and the provision of any needed follow-up services.
PacifiCare: Yes, at the plan level there is a 24-hour nurse line and medical audio library. Members can listen to pre-recorded health topics or speak with a licensed registered nurse. The nurse line staff can provide general counseling and triage recommendations. At the PMG/IPA level, PCPs are contractually required to provide after hours call coverage.
35. Do you include treatment by a physician’s assistant (PA) or nurse practitioner (NP), rather than by a physician? Do you guarantee a physician exam for adults when requested by the patient?
Aetna: Yes, but physicians using PAs or NPs are required to oversee services. Members have a right to request a PCP.
Anthem Blue Cross: Treatment by a physician’s assistant or nurse practitioner is included in our coverage, if available at the PMG/IPA level. Members always have the right to see a physician, rather than a PA or NP, if desired.
Cigna: Yes, when appropriate, physician’s assistants or nurse practitioners can work together with a physician. Yes, customers can request an annual physical examination.
Health Net of CA: As long as a physician’s assistant or nurse practitioner is under the physician’s guidance and providing treatments under the scope of his or her license, treatment is covered. Members have the right to have exams conducted by physicians rather than physician assistants or nurse practitioners.
Kaiser Permanente: Yes, members have the option to request treatment by a PCP, physician’s assistant (PA), or nurse practitioner (NP) when they are available and when medically appropriate. PAs and NPs are licensed health care practitioners who work in a variety of specialties, including pediatrics, obstetrics/gynecology, cardiology, pulmonary medicine, and gastroenterology.
PacifiCare: Yes, treatments by Physician’s Assistant (PA) and Nurse Practitioner (NP) are included. However, the member has the right to request a physician examination.
36. Can doctors be terminated for over utilizing services?
Aetna: When inappropriate use of services, under/overutilization or quality issues are identified, the provider is counseled; an action plan for improvement is developed; and service activity is monitored. The provider could be terminated if performance does not improve.
Anthem Blue Cross: Anthem contracts with the PMGs/IPAs, which contract with the individual providers. If a physician does not correct inappropriate utilization after counseling, they may be subject to discipline, including possible termination, by either the PMG/IPA or Anthem Blue Cross.
Cigna: Cigna has never terminated a physician’s contract for over utilizing services unless there was evidence that it was hurting the quality of care or was fraudulent.
Health Net of CA: A Health Net peer review team measures and rates adverse action material submitted by providers and various primary source agencies, including the Medical Board of California, the National Practitioner Data Bank, the Healthcare Integrity and Protection Data Bank, Medicare/Medicaid Sanctions, Office of Inspector General, opt-out Medicare reporting, and the claims history for credentialing and re-credentialing. Health Net also investigates allegations made in the community and by the media. The provider has a right to appeal the decision through a fair hearing. Health Net uses quality data in physician management and evaluation to help identify potential provider issues.
Kaiser Permanente: Our integrated health care system ensures that not only our doctors, but also our entire network functions at optimal efficiency to manage utilization by implementing best practices. Outcomes from HEDIS and internal utilization reports are available online to doctors and administrators to help them assess appropriate care and access levels, capture long-term performance trends, and identify areas of potential over utilization and underutilization. Utilization reports are also used to drive improvements in quality, access, and member services that result in improved outcomes, increased member satisfaction, and lower costs. Exceptions to best practice guidelines are identified, investigated, and corrected as needed.
PacifiCare: Yes. We have terminated a small number of contracts with participating practitioners as well as delegated providers for failing to adhere to quality standards, typically less than one percent annually. The precipitating events included behavior presenting a potential risk of imminent harm to PacifiCare members and behavior contrary to the requirements of state and federal law. Our termination procedures adhere to contractual and regulatory requirements, and include informing the provider with required appeal rights and description of the appeal process.
37. How do you determine with which providers to contract? Do providers get incentives for refusing to contract with other plans (for example, to maintain a semi-exclusive relationship with a managed care plan)?
Aetna: It is monitored based on geographic access with the necessary mix of physician specialties and hospital services. An annual study determines the availability of PCPs relative to residence of member population. Providers don’t get incentives for refusing to contract with other plans.
Anthem Blue Cross: We consider geographic factors, experience of PCPs and specialists, board certification, and quality/reputation factors. We do not provide incentives for refusing to contract with other health plans.
Cigna: Contracting is based on geographic, business, and customer needs. Health care professionals must meet credentialing criteria including verification of education and license status. There are no exclusive or semi-exclusive relationships.
Health Net of CA: To ensure the quality of the Health Net network, all potential Participating Physician Groups (PPGs) are subjected to intensive reviews to ensure they meet or exceed Health Net’s guidelines in the areas of medical management, financial viability and stability, and network accessibility. No incentives are given for refusing to contract with other plans.
Kaiser Permanente: Kaiser Foundation Health Plan (KFHP) contracts exclusively with the Permanente Medical Groups in Northern and Southern California to provide comprehensive medical services to members including primary care, specialty care, laboratory, and imaging services. Our doctors do not contract with other plans. On occasion we will contract health care services from doctors, usually specialists, who are required by their contracts to provide the same high-level of medical and personal service as that from our own internal doctors.
PacifiCare: Once we determine that network expansion is necessary, we research available providers in that area. We contact prospective providers for detailed assessments on their credentialing, quality assurance, and administrative capabilities. Before contracting, we assess area needs and hold initial discussions to gauge mutual interest. If this initial assessment is satisfactory, a provider delivery systems team begins contract negotiations. The length of the process varies depending on the urgency of need for additional providers and the availability of these providers during the auditing and contracting process. The process usually takes from two to six months. We do not offer anti-competitive incentives to any physician.
38. How can a member get information about a doctor’s schooling and malpractice suits?
Aetna: Plan service professionals have access to the plan’s national provider database, which generally includes the medical school of graduation; also members can view DocFind, our online provider directory at www.aetna.com. Malpractice information is not available.
Anthem Blue Cross: Members can get information about a doctor’s board certification status on the Anthem Blue Cross ProviderFinder directory web-based tool. Members can also request information about a doctor’s malpractice and schooling from the Medical Board of California via the Website, phone, in writing or they can contact the PMG/IPA directly. Also, they can call the Medical Board of California for malpractice information.
Cigna: Customers can call our customer service department or look up the information on myCIGNA.com. Malpractice information is available to the public through the state medical board website. A peer review committee, staffed by Cigna-employed doctors and non-employed doctors, reviews individual physicians’ histories before credentialing and re-credentialing the physician into the Cigna network
Health Net of CA: Members may contact Health Net’s Customer Contact Center to get information about a participating physician’s schooling. Members may also access Provider Search at www.healthnet.com for physician languages, board certification information, provider-specific information, and weekly or daily provider updates. Members may contact the Medical Board of California, the American Medical Association, or the applicable specialty board for information about a doctor’s malpractice suits.
Kaiser Permanente: Each medical center maintains physician information, which members can access to verify licensure, medical school graduation, residency, and fellowship training, and board certification. Members can also find physician bios and background information at kp.org and can also contact the California Medical Association for malpractice information on any doctor.
PacifiCare: The member can call customer service for educational history, licensing information and board certification. The member can call the Medical Board of California for malpractice information.
39. What are your grievance procedures?
Aetna: Our customer service professionals can respond to most issues by phone. If the issue cannot be resolved during the call, the customer service professional researches the inquiry and then responds to the member. Our goal is to respond to all inquiries in 15 business days. Members who are not satisfied with the response can file an oral or written grievance. We will forward a written notice stating the result of the review to the member in 30 business days of receiving the grievance. The decision is final and binding unless, in 30 days, the member submits a written request of the notice of the grievance decision for a hearing by the hearing panel/grievance committee. The member’s next course of action is to request an external review. The external reviewer decides in 30 days of the request. Expedited reviews are available when a member’s physician certifies that a delay in service would jeopardize the member’s health. Once the review is complete, we abide by the decision of the external reviewer. The Complaints and Appeals Tracking System was developed to support our national grievances and appeals process.
Anthem Blue Cross: Anthem is responsible for registering, investigating, and responding to member grievances and appeals. The appeal process is not delegated to the PMGs/IPAs. To file a grievance and appeal, the member should call the toll-free Anthem Blue Cross customer service number listed on their ID card or they can also submit a grievance in writing to the Anthem Blue Cross Grievance and Appeals P.O. Box. Members can also file an appeal or grievance online atwww.anthem.com/ca. After we review the member’s grievance and appeal, the member receives a written statement of the resolution within 30 calendar days. The member has the right to request an expedited appeal if their condition is acute or urgent. Expedited appeals are resolved within three calendar days.
Cigna: Customers can call our customer service department or file a written complaint appeal. The complaint is investigated and reviewed in 30 days (when appropriate) and the customer is notified of the decision. An expedited appeal can be filed when the individual or health care professional is concerned with potential loss of life or health or the ability to gain maximum function. When necessary, procedures are modified to meet or exceed applicable regulatory and accreditation guidelines.
Health Net of CA: When members complain about the quality of service provided by the plan or its participating practitioner, the grievance is documented and researched and an acknowledgement letter to the member is sent within five days. The hospital/ PPG/practitioner has seven days to respond to the grievance. The final resolution letter will be sent to the hospital/PPG/practitioner. If it takes longer than 30 days to resolve, a letter of explanation will be sent to the member. The grievance is documented when members complain about the direct provision of care or the quality of care by a participating practitioner. If the matter is urgent, it will be forwarded to a clinical specialist for immediate attention and resolution (if required, care will be provided to the member). An acknowledgement letter and medical records release form will be sent to the member within five days. The hospital/PPG/practitioner has seven days to respond to the grievance. Health Net will determine if the grievance can be resolved with the records at hand if the member does not provide out-of-plan records or if the medical record release form is not signed. If it can’t, the case is closed until all necessary information is provided. After review, a letter to the member will communicate the disposition. The final resolution letter will be sent to the hospital/PPG/practitioner. If the matter takes longer than 30 days to resolve, a letter will be sent to the member to explain the delay and provide an estimated resolution date.
Kaiser Permanente: Our members can submit complaints to the member service representative at each medical facility and through the Member Services Call Center. Complaints are acknowledged within seven calendar days and a response made within 30 days. Our goal is for a complaint or grievance to be resolved within 60 days from the date it was received. An external, independent, third party review process is available to non-Medicare members who have completed the internal grievance/appeals process.
PacifiCare: Our top priority is for members to receive the services they need. If a problem occurs we encourage members to contact our Customer Service department as their first source for resolution. This team will make every effort to find a solution to the member’s situation. If the situation requires additional action, the member may submit a formal complaint requesting an appeal or quality review. The following is a summary of our formal process for appealing a health care decision. The member must submit a grievance in writing within 180 days of the initial decision to: PacifiCare of California Appeals and Grievance Department. Additionally, members in California may file an appeal using the online grievance form available at www.pacificare.com.
40. What systems are in place for assessing participant satisfaction?
Aetna: Member satisfaction is measured yearly at the network level using CAHPS 2.0H survey. The plan administers the most recent survey required by HEDIS to assess satisfaction. We also participate in the Consumer Assessment Survey to evaluate member satisfaction with IPA and Medical Groups.
Anthem Blue Cross: We conduct a variety of surveys each year to measure our members’ health and satisfaction to improve the quality of care and customer service. Each year, Anthem collects feedback from the various constituents that impact our business. We listen to all customer groups (members, employers, health care providers and insurance agents/brokers) and take into account the entire health care experience. Our research efforts provide us with a glimpse into the minds of our customers, telling us how best to deliver superior quality and service. We look at the experience through their eyes. We also collect feedback from our members and providers on an ongoing basis to get an even deeper look at the service experience. A key component of this ongoing survey program is the diagnosis and root cause analysis performed on each call where the surveyed member was neutral or negative about his experience. We use the Member and Provider Call Center Transaction Survey Programs as part of our strategy to improve customer satisfaction. The survey obtains solid, actionable operational-level measures of our customers’ needs and an evaluation of our performance at all key touch points. More than 100,000 surveys are conducted with members annually.
Cigna: Cigna uses the Consumer Assessment of Healthcare Providers and Systems (CAHPS) customer satisfaction survey, which ask consumers and patients to report on and evaluate their experiences with health care. It includes measuring satisfaction with medical groups and addresses utilization management, appointment wait times, office staff, etc. We continually monitor and work to improve customer satisfaction.
Health Net of CA: Health Net offers customer support and satisfaction surveys for members, providers, employer clients, and brokers. Health Net also participates in the annual National Committee of Quality Assurance (NCQA), HEDIS, CAHPS surveys and the Decision Power (disease management program) Satisfaction Survey. These reports are available to employer groups upon request. Additionally, Health Net conducts satisfaction surveys within our consultant and broker networks to ensure that we are meeting the needs of our clients. Health Net’s Customer Contact Center has implemented a post-call survey for all callers (members, providers, employers, and brokers) across all lines of business (Commercial, Medicare, and Medicaid). The survey, which is conducted periodically throughout the year, provides Health Net with valuable insight using the voice of the customer to measure amount of caller effort required to resolve issue, first call resolution, overall satisfaction with service provided, and how likely they are to recommend Health Net to a friend or family member.
Kaiser Permanente: We conduct ongoing surveys to evaluate member and patient satisfaction with doctors, access to services, and quality of care. Survey feedback is disseminated throughout the organization to target areas for improvement.
PacifiCare: PacifiCare uses the NCQA CAHPS annually to assess patient satisfaction with their care. Our satisfaction results are reported in our annual HEDIS results. CAHPS is a mail survey, which fulfills a component of the NCQA accreditation process. A telephone follow-up and interview occurs among non-responders per NCQA specifications.
41. Do you participate in outcomes research? Do you provide physician performance review data to the public?
Aetna: Yes, HEDIS is available for public review through the California Cooperative HEDIS Reporting Initiative.
Anthem Blue Cross: Yes, we have tools that support predictive modeling, provider profiling, hospital profiling, disease management, network analysis, quality assessment, regulatory reporting, and HEDIS submission. Additionally, Anthem has acquired HealthCore Inc., a leading outcomes research company. Performance review data for our PMGs/IPAs is available publicly on our website and in provider directories.
Cigna: Cigna is accredited by NCQA and participates in reporting HEDIS clinical outcome data, which is available for public review. Cigna also participates in the Integrated HealthCare Association’s Pay for Performance program. It provides data at the medical group level, which is reported to the public annually through the state’s Office of the Patient Advocate. Cigna also participates in the California HealthCare Foundation’s CHART hospital quality initiative. Through myCIGNA.com, the company offers an array of information to customers about the quality of health care professionals and facilities.
Health Net of CA: Medical groups are rated on wide-ranging quality-of-service and quality-of-care measurements. Results are available at www.healthnet.com, where members can view the Hospital Comparison Report and Participating Physician Group Report on a number of quality-of-care and service measures.
Kaiser Permanente: The most recent developments in medical outcomes research are incorporated into our evidence-based Clinical Practice Guideline program, assessed by our New Technologies Committee, and incorporated into our extensive library system with online capabilities. In addition, our clinicians are involved in a broad scope of clinical, epidemiological, and health services research projects. We earned ratings of Excellent in the latest review by the National Committee for Quality Assurance and routinely earn high scores in outcomes based surveys, such as HEDIS, Leapfrog, and METEOR, which measures our member satisfaction.
PacifiCare: Yes. Outcome results are incorporated into our provider group profile, which compares each provider group with network averages. We release these performance results to the public through our quality index profiles. The reports look at clinical, service and administrative quality measures. PacifiCare motivates provider compliance by intervening aggressively when deficiencies are found and by sharing best practices when excellence is identified.
42. Do you notify members when their PCP is no longer a member of the plan? How?
Aetna: Yes, members are notified by letter. They are apprised of transition of care issues and instructed on how to select a new PCP.
Anthem Blue Cross: Yes, PMGs/IPAs are required to provide 90 days notice to the plan when a physician within the PMG/IPA leaves the group or is terminated from our network. The PMG/IPA must offer the services of another PCP within the group. The plan provides at least 60 days’ notice in writing to all members enrolled with the terminating PCP. This letter includes the name of their new PCP or medical group.
Cigna: If a PCP is no longer a network physician in our plan, customers are notified by mail about 60 days before the effective date of the change and are encouraged to choose a new PCP.
Health Net of CA: Health Net Participating Physician Groups and individually contracted physicians are required, by contract, to notify us of any changes to the provider network including new physicians joining the PPG, address and telephone number changes, and physician terminations. Health Net notifies members when their PCP leaves the network or becomes affiliated with a different contracting PPG. Members can follow their PCP to a new contracting PPG. Members can choose a new PCP within the network or remain with their PPG if their PCP is no longer available in our network. When possible, members will receive a written notice within 30 to 60 days of the provider’s decision to leave the network. Provider listings are available at www.healthnet.com and are updated daily.
Kaiser Permanente: Yes, each medical center has developed general protocols to facilitate the transition of care to another doctor. Members assigned to a PCP are provided notice of the PCP’s departure 60 days in advance when possible. Members who are scheduled to see the physician for outpatient care are contacted to reschedule with another plan doctor if prior notice to a member is not able to be provided due to timing of the physician’s departure.
PacifiCare: Yes, PacifiCare sends a notification letter to all affected members 30 days prior to the termination date of a physician or medical group. The member selects a new PCP or medical group. If the member does not select a PCP or medical group within 30 days, we automatically assign a PCP or medical group that is geographically closest to their residence. If the member is unhappy with the assigned provider, he or she may request a change at any time by calling customer service.
43. What action is the plan or the IPA/MG taking to have online eligibility, administrative changes, referrals, etc?
Aetna: We participate in the Work Group for Electronic Data Inter-change, the Computerized Patient Record Institute, and the American National Standards Institute. A monthly eligibility file is provided to IPAs and Medical Groups.
Anthem Blue Cross: Through our Internet application, Employer-Access.com, group administrators can process eligibility transactions including additions, changes, and cancellations. (Changes are processed in real-time, assuming a confirmation response is received.) The administrator can also order ID cards; perform quick inquiries on employees; and locate providers via our provider finder. The “EmployerAccess.com” application features confidential and secure data through user ID and personal identification numbers, drop-down menus for easy point-and-click operation, and easy to follow hyper-link steps to guide the administrator through electronic enrollment, benefit changes, and maintenance processes.
Cigna: Cigna recently enhanced our website for health care professionals, offering easy access to online eligibility, detailed benefit information, claims tracking, and a new claim coding disclosure tool, which offers an immediate response to inquiries. For customers, myCIGNA.com offers online eligibility tools, claims support, and other tools that allow people to select or change their PCP and get personalized medical information and quality data about health care professionals. In addition, CignaAccess.com provides a single point of access to online tools and services to help make benefits administration easier. CignaAccess.com is a resource for employers in employee support, benefits administration, and security administration.
Health Net of CA: At www.healthnet.com, providers, members, employers, and brokers can perform wide-ranging administrative functions, including eligibility verification. Health Net uses the Internet to help employer groups make processing eligibility changes and pay bills. It is a free service to employer groups. Employer groups can log onto www.healthnet.com or eServices.healthnet.com. For brokers, Health Net’s Broker Solutions site provides online applications, product and rate information, provider directories, email access, and more. Providers can view mem-
ber eligibility, copays, medical policies, claim status, authorization status, and more. Members can access secure information about their coverage, correspond with Member Services, order ID cards and forms, file grievances, change addresses, check eligibility/benefits, change PCPs/ PPGs, view a pharmacy drug list, search for providers, look up information for their specific needs, get pharmacy refills, and more. Members can also connect to their www.healthnet.com online account via Health Net Mobile. Available free on Apple, Android, BlackBerry and other web-enabled devices, members can use this application to quickly conduct a wide variety of business transactions with Health Net at the push of a button.
Kaiser Permanente: Eligibility files are processed by our extensive online system maintained by our California Service Center in San Diego. Account representatives update membership online via electronic media files from purchasers. Nightly bulk transmissions from all claims and membership systems supply membership eligibility information to other clinical systems as needed.
PacifiCare: PacifiCare providers can check eligibility and claim status; print common forms; and view the specialty referral list at www.pacificare.com. We offer a paper and electronic referral process. In California, providers can access iExchange via the Web for electronic preauthorization requests and hospital admission notifications. The process varies for networks that are delegated and managed by contracted providers. Some providers have electronic referral systems in their own specialist network and others use paper submission. We do not track electronic referrals for these providers since they track these statistics internally.
44. How has your plan changed from last year?
Aetna: Our CA HMO plan now reflects all PPACA/HCR requirements.
Cigna: Several provisions of the Affordable Care Act have gone into effect for non-grandfathered plans, and so our plans have changed to be in compliance with the new law. More information is available on our “Informed on Reform” website on Cigna.com, including FAQs for brokers, employers and customers. In addition, Cigna has been very active and a leader nationally since 2008 in working with health care professionals to establish collaborative accountable care programs that seek to expand patient access to health care, improve care coordination, and achieve the “triple aim” of improved health outcomes (quality), lower total medical costs and increased patient satisfaction. We have partnerships that are showing very positive results, and we recently launched our first collaborative accountable care program in California. Including this program, Cigna is now engaged in 32 collaborative accountable care initiatives in 16 states, encompassing more than 300,000 Cigna customers and more than 4,500 primary care physicians. We have a goal to have 100 collaborative accountable care programs with 1 million customers in place by the end of 2014.
Health Net: Health Net is planning to upgrade our Customer Service Center’s systems and capabilities. This includes integration and expansion of Health Net’s Interactive Voice Response, web and mobile self-service capabilities. The goal of this project is to eliminate non-value-added manual effort and to insure consistent and accurate customer experience regardless of the channel accessed. Health Net is rolling out a new customer service management tool that will assist in contact management, thus making it easier for our staff to facilitate inquires and provide accurate, timely and consistent customer interactions. The new application delivers the ultimate customer experience by providing a single integrated desktop and a consistent workflow across our lines of business. The new system also automatically logs all call notes.
Health Net is successfully promoting culturally appropriate services that reduce health care disparities. In January 2012, Health Net received a National Committee for Quality Assurance (NCQA) Multicultural Health Care (MHC) Distinction. This coveted distinction sets Health Net of California apart from other health plans in that it is only awarded to high quality “organizations that engage in efforts to improve culturally and linguistically appropriate services and reduce health care disparities.” Health Net is the first health plan to receive the distinction for our Medi-Cal line of business and for both Medicaid and commercial lines of business (including our Healthy Families Program business). To date, only seven other health plans across the U.S. have received the distinction. The Distinction is valid for two years. To maintain the Distinction, Health Net must resubmit before the end of the second year.
On April 2, 2012, Health Net, Inc. announced that its subsidiary, Health Net Life Insurance Company, completed the sale of its Medicare stand-alone Prescription Drug Plan (Medicare PDP) business to a subsidiary of CVS Caremark. Health Net will continue to provide prescription drug plans as part of its Medicare Advantage plan offerings.
Kaiser Permanente: Significant changes were made with our plan in 2012 and are expected in 2013. We made several preventive services for women available without the need for a copay, including annual well-woman exam, family planning counseling, breastfeeding support, supplies, and counseling, gestational diabetes screening, domestic violence screening and counseling, human papillomavirus (HPV) testing, sexually transmitted disease counseling, and HIV screening and counseling (certain religious groups may be exempt from covering contraceptive methods and counseling). Medically necessary behavioral health treatment for autism spectrum disorders (ASD), including autistic disorder, Asperger’s syndrome, and pervasive developmental disorder – not otherwise specified are covered. We are expanding our contracted network to include qualified autism service providers, so we can offer members the newly required behavioral health treatment. New and upgraded medical facilities opening in 2012-2013 include the following:
San Mateo Medical Offices (2012)
South Sacramento Medical Center (2012)
Antelope Valley Medical Offices (2012)
Chester Avenue Medical Offices, Bakersfield (2012)
Ontario Medical Center (2012)
Garfield Specialty Center, San Diego (2012)
South Los Angeles Medical Offices (2012)
Orange County-Anaheim Medical Center (2012)
Palomar Medical Center West, Escondido (2012)
Indio medical offices (2012)
Lake Forest medical office building (2012)
Iris II medical office, Moreno Valley (2012)
San Diego medical center expansion, San Diego (2012)
San Marcos medical offices (2012)
Thousand Oaks medical facility (2012)
Tustin Ranch medical office building (2012)
Ventura behavioral health center (2012)
Carmel Valley medical offices (2013)
Fontana Medical Center (2013)
PacifiCare: There are no significant changes to the general plan structure from last year; however, there is flexibility on how plans are quoted. Clients requesting customization work closely with their broker to determine the best possible options for their company.
Self-Funding–Self Funding in 2013 with the Affordable Care Act
by Mark Reynolds, RHU
Everyone has heard of Einstein’s theory on insanity in which you do the same thing over and over, etc, etc. Well, here is a new definition of insanity to consider. I could argue that agreeing to write an article about self-funding group health plans in an era of unpopular health care reform to be published in a prominent industry magazine just a few weeks before a presidential election could be the new definition of insanity. Granted, it may not grow to be as popular as Albert’s definition, but one would probably agree that it is pretty much crazy.
Be that as it may, it is important that we all consider what the results of the election may bring to health plans, the decisions that employers face in 2013, and the impact we all can make by embracing an alternative to the limits and restrictions of fully insured plans. Health plans of all types are under siege by the public and by politicians, but that’s why brokers must view this point in time as an opportunity to make a difference for employers and their employees.
This is Not the First Time We’ve Seen Health Care Reform
Reforming the way health care is financed and delivered started back in the 1940s and resurfaced again, in a big way, in the 1960s with the passage of the Medicare Act. Each decade has brought some effort and legislation to reform or simply change some aspect of health care: the HMO Act and ERISA in the 1970s, COBRA in the 1980s, AB 1672 and HIPPA in the 1990s, Medicare Part D, and HSAs in the 2000s, leading to the attempted takeover or the so-called overhaul of health care in 2010 by the Affordable Care Act (ACA).
One thing many of these efforts have in common is that, even if the intent was good, health care cost eventually began to increase at unsustainable rates; the public reacted; and the market responded. Often, the market’s response to control cost was to implement self-funded plans. The market always responded and it will again whether it be full on ERISA-based self-funded plans with reinsurance or the popular HRAs and MERPs with fully insured HDHPs. So what should we plan for and how should we plan for it?
The Next 15 Months Will Bring Unprecedented Opportunity
First, let’s frame the situation. At least two facts are certain: employers have seen their plan costs increase dramatically over the past seven years and employers are searching for relief. Over the past several years, many brokers supplied that relief by helping employers strip down their plans with leaner benefits, higher copays, and coinsurance as well as much higher out-of-pocket costs. Some brokers implemented HSAs to help, but when the employer stopped funding the HSA, these plans became just high deductible health plans.
The second certainty is that, come mid-2013, employers will face a fundamental decision about the core benefits they provide for their employees. As employers start to realize the inevitability of ACA in 2014, they will ask themselves, “Do I continue to provide benefits or give them up and pay the penalty?”
One choice the employer may make is to continue offering benefits. This maintains the employer’s culture of providing benefits for that extended family known as employees. Traditionally, employers started offering benefits to attract and keep good employees but, over time, company benefit plans have become a part of a company’s culture. Employees count on them and they plan around them. It is easy for employees because they don’t have to search out a broker, a carrier, a plan, or PPO. Most employees have grown to appreciate the culture of benefits that their employer provides. This comfort level has led many to an entitlement mentality; the fact remains that employer provided benefits were and are easier for employees.
The other decision the employer may make is to stop providing benefits. This leaves employees on their own, which may lead to no coverage simply because it may be the first time the employees have had to make this decision on their own. If employees are forced to start selecting and paying for health insurance on their own, it will be confusing and many will not make the effort. Plus, even with the subsidies promised for qualified employees, the cost will push employees away from coverage because most now pay very little or nothing to get their benefits. Many will not want to pay for it and may think they don’t need to buy it. Of course, this second decision could lead many brokers to see their years of work building their agency and their hard-earned income vanish within months. It may sound Draconian or far-fetched now, but the decision employers will face is real. Employers will either decide to keep their plans or discontinue their plans based on the solutions that brokers provide. That means their decision will be based on the quality of the information that a broker provides. The key is how brokers will position themselves so that the employer chooses wisely and maintains that employer-based, family-oriented tradition of providing a solid health plan that employees appreciate.
The Broker’s Role
You have read, many times, that the ACA will require brokers to perform more as consultants than ever before. This may sound somewhat trite, but it is true. Consider, for a moment, the information that employers will need in order to face the decision I outlined earlier. Employers will have questions about following: the Exchange, penalties for employers and employees, how part-time staff are addressed, the associated cost, essential benefits, etc, etc.
But most important of all, employers will want to know if there is any possible way to maintain their own high quality benefit packages, lower their costs, and avoid disrupting their business. These questions address a core concern for the employer: How does the employer retain its experienced staff if it no longer provides benefits?
Some morning, sit with a pad and pen and think up the questions and resulting scenarios that employer will face in 2013. When you finish, you will come to the conclusion that employers will need a good insurance consultant more than ever. Then ask yourself, “Am I a good consultant and how do I compete against others in my region?”
Embracing Self Funding Will Set You Apart
Anyone can be a broker with spreadsheet proposals. I don’t mean to sound critical, but you know that most brokers get their proposals from just a few sources, so the proposals do nothing to help differentiate a broker from competitors. One fully insured plan is and will probably continue to be built and priced just like every other fully insured plan in the market. Carriers have been very creative over the past 10 years and they will continue to do their best to meet the market’s needs. But, restrictions and guidelines within ACA will limit much of what a carrier can do. So how can you be different?
As the subtitle suggests, embrace self-funding. By this, I mean that brokers can’t just say they support self-funding; they must focus their business practice on HRAs, MERPs, and traditional self-funded plans. Today, without the employers’ knowledge, many brokers prequalify their groups, determining that self-funding would not work. This leaves the broker-of-record exposed to competing brokers who will present self-funding to every employer, even those with as few as two employees.
Equally important is that brokers should find an experienced carrier or TPA partner that can provide the foundation for the plans the broker will market. A qualified TPA or carrier partner will provide that extra boost that a broker needs to be different; to get the employer’s attention; and most importantly, to help the employer maintain the benefit package it needs to preserve the employer’s advantage in its market space.
There Is Time and There Is Opportunity
Regardless of the election results this November, brokers can count on a couple of things.
One is that employers will still want to provide health benefits for employees because not providing them could disrupt the business and because it will remain a good tool to recruit and retain key staff. The second thing to count on is that employers will continue to be unhappy with their benefit plans from both a price and benefit perspective. Who would be happy with a $750 deductible, a scaled-down network, a value-savings-whatever plan with $250 to $500 brand Rx deductibles, out-of-pocket costs that bankrupt the average employee, and premiums that are beyond the average employee’s ability to pay?
So, regardless of election outcome, brokers can prosper by embracing self-funding as a solution and mastering the presentation that’s required to educate employers about this option. Employers will be seeking solutions to their own business needs. They face immense uncertainty within their own industries, with new levels of regulations and government intervention. Because of the unknowns that employers face, they often feel that making no decision is better than making a bad decision. Brokers who focus on self-funded plans will be able to educate employers about new solutions to help the employer maintain the integrity of its core business benefits.
Brokers who prepare for this opportunity must seek the partners they will need to meet the needs of clients and prospects. A little preparation now can catapult brokers into a new generation for their agency and they will see their business grow and thrive while many others sit and wonder. Brokers who adapt to a self-funded, solution-based marketing approach that actively markets for business can prosper while providing real solutions for employers.
–––––––––
Mark Reynolds is a member of the Team at BEN-E-LECT. BEN-E-LECT’s trademarked Employer Driven Health Plan model provides MERPs, HRAs, and Self-funded plans to thousands of employers throughout California and the Southwest United States. BEN-E-LECT’s ERISA or E-Based health plans help employers, with 2,500 employees, lower and control the cost of their group health plans. BEN-E-LECT’s corporate office is located in Visalia, Calif. Mark can be reached directly at 559-250-2000 or markr@benelect.com.
Self-Funding–Three Reasons To Stay Self-Funded Since the Affordable Care Act
by David Zanze
The Affordable Care Act requires more robust health benefit coverage for all health plans. But self-funded employers will be immune to the same unsubstantiated rate increases and higher premiums that will plague fully ensured employers. Your client would save more by staying or becoming self-funded.
Make no bones about it; employers will spend more on healthcare expenses for employees. But self-funded employers will be better situated to control the effects of this sweeping healthcare legislation. Here are three reasons why:
1. Fully Insured Carriers are Taking on More Risks That They Cannot Shift and they Are Not as Motivated to Control Costs
Under the Affordable Care Act, insurers have dramatically higher exposure to risk without the ability to include rate adjustment factors for health conditions or demographics. New community rating rules limit the insurance carriers’ ability to charge higher premiums for older, riskier individuals and small groups. Also, the health insurance game has become more expensive and riskier for insurers now that certain risk reduction strategies are not allowed, such as lifetime and annual limits and exclusions for pre-existing conditions. Carriers are being squeezed on all sides by the law and accompanying regulations.
These costs will be passed onto the consumer, at least to the extent that insurers can pass on the costs. Employers will pay higher fixed monthly premiums for fully insured policies. Carriers are now required to give back “excess” premium dollars in the form of medical loss ratio reimbursements.
Of course, fully insured health plans will meet all the new requirements so that the insurance carriers can sell their products in the marketplace, but carriers do not have a vested interest in the consumer. There will be no price pressures to keep costs low other than competition among rival carriers. Try as it might, the California Department of Insurance does not have the authority to regulate rate increases. It’s still an open market. Qualifying for California’s November 2014 ballot is an initiative to regulate the rates that health insurers can charge. But even this attempt at rate reform would be no panacea for large groups since it would only apply to individual and small group health insurance markets.
Likewise, the Affordable Care Act has no mandates requiring insurance carriers to provide affordable health benefit plans to the average consumer. Regulators will not be able to prevent inflated prices and unsubstantiated rate increases. The only incentive to keep prices down will be to attract and retain current clients.
The individual mandate does force more lives into the system since consumers will be required to purchase health insurance or pay a penalty. The demand will be great and so will the supply, but the future cost of health benefits is anyone’s guess. The California healthcare exchange will provide options, but there is no guarantee that they will be affordable or cost-effective.
2. Self-Funding is in the Employer’s Self-Interest and Provides Incentives to Keep Costs Down
For self funded employers, their own financial interests remain at the forefront. There are some fixed costs of administering a self-funded healthcare plan, such as claims processing, stop loss premiums, and administrative fees. But self-funded employers only pay the direct costs of administering employee claims. In contrast, conventional insurance premiums compensate for overhead, profits, and commissions. If the employee base is relatively healthy, having a self-funded plan can be one of the best ways to manage the rising costs of healthcare. Like a fully insured plan, a self-funded plan is subject to many Affordable Care Act reforms, such as having minimum essential coverage requirements and prohibiting exclusions for pre-existing conditions and annual and lifetime limits on essential benefits. But only fully insured carriers will be subject to California state law. As California continues to legislate costly new benefit requirements, self-funded employers will not be subject to this legislation.
3. Self-Funding is Customizable and Controllable
The costs of fully insured plans are unpredictable for employers since carriers have control over monitoring employee health and underwriting for risk. With fully insured plans, employers don’t have access to employee health claims.
A significant advantage of a self-funded plan is that employers do have access to employee health data, which drives customizable, cost-containment programs. TPAs provide various reports on claims spending and utilization, which allow the employer to analyze the overall health and utilization of the plan. The employer can revise or reinforce components of the plan to meet the needs of the employer and plan participants. Based on healthcare data, self-funded employers can determine the health of their populations and control costs by implementing HIPAA wellness, disease management, and case management programs. Employers also have the control and flexibility to design their own health plans.
In conclusion, the Patient Protection and Affordable Care Act has changed the healthcare landscape. But amid the changes, your self-funded client will be better positioned to save on healthcare costs while providing a quality health benefit plan that meets or even exceeds the requirements of the Affordable Care Act. That is instead of padding the pockets of insurance carriers that may or may not have their client’s best interests at heart.
–––––––––
David Zanze has nearly 30 years experience serving as a leader and innovator in the healthcare industry. He joined Pinnacle Claims Management Inc. as president in 1996. Pinnacle Claims Management, Inc. (Pinnacle) is an all-inclusive health benefits third party administrator (TPA) that offers competitive, cost efficient claims management in tandem with the latest technology. Pinnacle administers benefits for a diverse range of small to large sized employer groups from all business sectors of the marketplace. For more information, call 866-930-7264 or visit www.pinnacletpa.com.
Long-Term Care – How to Discuss Long-Term Care Insurance vs. Self-Insuring with Clients
By Steve Cain, EVP
After each quarterly LIMRA report is released, I usually discuss it with my life, P&C and employee/executive benefits colleagues. It is clear that the long-term care insurance (LTCi) industry has struggled to increase market penetration for the masses. Part of the problem may be the way agents are positioning this issue.
Over the years, the sale of LTCi mainly focused on selling a health insurance product vs. selling the concept of Long-Term Care planning. LTCi, previously viewed as a senior market product, has now become a Boomer market product, and according to AALTCI the average purchase age in 2011 was 57 years old. In order to reach and communicate effectively with a different consumer than originally targeted, the conversation has to be elevated or changed.
Thanks to advances in medicine, exercise and better diets, Americans are living much longer and fuller lives. But the fact that we are living longer requires a heightened focus on retirement planning. I am suggesting that distributors (insurance agents, financial advisors, CPAs, P&C and benefit brokers) lead the LTCi discussion with planning vs. product. The product is just the vehicle to help a client accomplish the goal of mitigating potential long-term care risk. Yes—LTCi products can be complex, with numerous moving parts. However, if the sale of LTCi is conceptual, then it is less likely you will get tripped up in the nuances or LTCi jargon. Essentially, you are convincing the client to plan for their longevity, addressing this issue like all other risk in their lives. This strategy resonates with Baby Boomers and their advisors who look at their risk management planning and clients holistically.
I have had the good fortune of having great mentors in the life insurance, P&C, and benefits business. Each shared a similar conversation when managing risk in their respective discipline. As insurance and financial services professionals, we help clients identify, assess and mitigate risk. Specific to long-term care, one of the best approaches is educating clients about the need to plan for a long and full life. Extended healthcare is a financial risk to their portfolios, not to mention their post-retirement lifestyles. In this vein, I assess the funding options for the financial risk and discuss the client’s healthcare options (caregiving challenges). I urge clients to mitigate the risk by planning—sometimes that might include an insurance product (traditional LTCi or combination Life/LTCi) to hedge against the risk, and sometimes it does not.
The Risk Management Approach
Long-term care planning should be approached no differently than in P&C, benefits or financial planning. Discussing the issue from a risk management perspective can help remove emotion and allow clients to draw parallels from other risks in their lives. There are traditionally four ways to manage any risk (property, liability, portfolio, estate tax or healthcare):
Identifying the Risk:
• Almost seven out of 10 people turning age 65 today will experience, at some point in their lives, functional disability and will need some paid or unpaid help with basic daily living skills. On average, they will require such help for three years (3.7 years for women, 2.2 years for men).
• Of the average 65 year old American’s projected three years of lifetime need for long-term care, about two-thirds of that time would be spent at home and one-third in either a nursing home or assisted living facility.
• Formal long-term care services are expensive. While the costs for private nursing home care vary widely, they average about $87,235 per year for a single occupancy room and $78,110 per person for double occupancy. Assisted living costs average $41,724 annually. Home care costs approximately $20 per hour. Accordingly, 10 hours of weekly home care would cost $11,400 annually and eight hours of daily home care would cost $58,240 annually.
Risk Management Strategies:
a. Avoid – we cannot avoid the aging process. I am from Los Angeles and we try harder here than anywhere! But it happens.
b. Reduce – we cannot reduce the risk of an extended healthcare event. In fact, it is an interesting inverse relationship between your good health and habits today and the potential need for home health or facility care tomorrow. The better shape a person is in, the more likely he /she is to live a long life, which might result in one needing assistance.
c. Retain – simply stated it is self-insurance or taking on this risk. Self-insurance is a viable option for many and is worth discussing this option in detail with clients. Critical discussion items include the actual healthcare: determining who will be the primary caregivers, managing the event, monitoring the providers, adjusting the care as needed, etc. Managing a long-term care event takes more than money. Funding of a chronic disability should also be tackled. Where will the money come from in the event that the client needs care? Is the client liquid? Has the issue of capital gains taxes been discussed (state & federal)? If retention is the optimal solution, I would urge advisors to create a long-term care plan document that details how the care event is to be managed.
d. Transfer – hedging against the risk with insurance. The amount of insurance or type varies, but an individual looks to insurance to protect him/her from risk. For most clients, this objective conversation leads them to see that there are really only two ways to manage this risk—retain or transfer. That leads to an analysis of each option and the client making a decision with the advisors as to how to manage the risk.
It’s easy to see that there are only two ways people deal with risk. It can be retained or transferred. Ultimately, avoidance and reducing the risk are not viable options. Clients must choose whether to self-insure or transfer the risk. As an advisor, you must help them plan for and mitigate this risk. If a client is adamant about self-insuring, take the emotion out of the discussion and start a planning conversation to formalize a self-insure strategy. In addition to the questions listed in point C above, ask the client: Where will the money come from? Who will be the caregiver? How will the caregiver be monitored? From there, you can plan in a methodical and effective way.
There are, of course, many individuals may chose to transfer the risk and there are two viable ways to do this: fully insure the risk or co-insure the risk. When a person fully insures the risk, they purchase insurance to cover everything in the case of a long-term care event. A client can also choose to co-insure by purchasing coverage for a predicted 70% of care and select to self-insure the remaining 30%.
By establishing the valuable role of LTCi in safeguarding your client’s retirement—and helping them maintain the highest possible quality of life—the path to action becomes much clearer.
–––––––––
Steve Cain is Executive Vice President and Sales Leader at LTCI Partners, a brokerage general agency specializing in long-term care insurance. He can be reached at steve.cain@ltcipartners.com or (877) 949-4582 x237.
Premium Financing – Turning a Good Year Into a Great Year With Premium Financing
by Leila Morris
An agent may only sell two or three large life insurance cases in a year. So closing that one extra case can make the difference between having a good year and having a great year. Premium financing can tip the balance toward selling that large life insurance policy. Experts addressed premium-financing opportunities at Succession Capital Alliance’s fourth annual conference in Las Vegas in August. More than 100 advisors attended the two-day invitation-only event.
Julian Movsesian, MBA, president and founder of CMS and Succession Capital Alliance presented examples of how life insurance agents have used premium financing to address complicated planning strategies for their clients including estate planning; buy-sell agreements; key person coverage, as well as retirement income needs and concerns.
Premium financing is simply an alternative funding method to purchase a large life insurance policy, explains Michael Rothman, director of Institutional Alliances with Succession Capital Alliance. The client enters into a fully collateralized loan with the intention of holding the policy to maturity. Premium financing is used for life insurance policies with an average target premium of $350,000 and an average face value of $10 million.
A client may choose this unique form of leveraged financing to maintain their cash flow or avoid having to sell investments or real estate to pay premiums. A lack of cash flow is one of the biggest obstacles to purchasing a large life insurance policy, Rothman noted. Premium financing also offers favorable loan rates, fees, and spreads. Certain features make it less risky than other financing options. And the risks can be mitigated by structuring a case correctly.
Premium financing can address multiple needs for clients including life insurance/estate planning, retirement planning (cash-value accumulation), and business planning-buy/sell or key-man policies. High net worth clients often have multiple needs, Rothman noted. Hot button issues for clients are freeing up cash value, discounting the cash flow on premiums, and having a bigger death benefit.
Identifying Candidates for Premium Financing
So who is a candidate for premium financing? The client should have a net worth of at least $10 million (liquid or illiquid), have the necessary collateral, and have outstanding credit. The client should also want, need, and be able to afford the life insurance coverage that you are proposing without financing.
The ideal client for premium financing may be one you already have. Rothman suggests looking at your existing book of business for clients who are paying more than $100,000 in premiums with cash values over $250,000. “The best opportunity for a large life insurance case is the large life insurance case you sold in the past. The renewal process is a new opportunity to have a new sale or provide better value to the customer,” he said.
Presenting the Case
Financing large purchases is nothing new for many high net worth individuals. They are used to weighing the pros and cons of whether to pay cash or finance real estate transactions, business operations, and investment opportunities. In the same way they purchase other large assets, clients should have the opportunity to consider financing the premiums of a large life insurance policy, said Rothman. “Premium financing strategies create choices for high net worth clients and more choices mean more cases closed. You can also restructure existing insurance policies to free up cash value or increase the death benefit,” he said. Rothman notes the following downsides of not presenting premium financing as an option to a client who could benefit from it:
• The client does nothing because they feel that too much cash is needed to finance the policy.
• The client goes with a competitor who presents a premium financing option that is poorly designed.
• After the sale, the client asks why you didn’t tell them about premium financing, which opens the door to liability and surrenders.
• A client may consider premium financing for the following reasons:
• Leverage: The client purchases insurance to protect their estate, business, or retirement plan using discounted dollars (large death benefit versus small premium).
The client purchases insurance with discounted cash flow, paying less than the premium for the same death benefit.
• A higher return: The client expects a higher return on insurance than on their cash or other investments (tax-free benefits).
• Liquidity: The client does not have the cash flow to purchase a large policy or wants to use cash for other purposes.
• Arbitrage: The client can earn higher returns on investments than the bank charges in interest or higher than the policy-crediting rate.
Doing Your Homework
There is a lot more to premium financing than meets the eye, Rothman stressed. You need to develop a custom design for each client. Creating a customized premium finance package means looking at non-financed options, doing collateral analysis, and integrating the new insurance policy with existing life insurance planning. In fact, you need to do a complete analysis of all of the options and of the client’s financials before designing and presenting a case to the client.
“You don’t want to be in a situation in which you present a $20 million illustration to the client and he decides to buy term insurance because the premium is too high. At that point, the case is damaged,” Rothman added. When designing a case, you need to underwrite the correct death benefit, have proper placement within jumbo limits, and achieve product diversification. Medical underwriting must be done before the loan is submitted. You also need to complete the client’s credit underwriting.
Rothman stressed that an agent needs to answer the following questions when evaluating a client for premium financing:
• What are their financials?
• What is their net worth and income?
• How are their assets held?
• Do they have the cash flow for a new plan?
• What are their sources of collateral?
• Have they done prior planning?
• Who sold insurance to them in the past?
• For the policy they are considering, what type of product and carrier is it? What is the planned premium, what is the death benefit, and what is the cash-surrender
value?
The following points are essential to designing a case:
• Benchmarking of non-financed versus financed premiums.
• Collateral/cash flow.
• Exit strategies and flexibility.
• An analysis of interest-rate sensitivity.
• Medical underwriting.
• Credit underwriting.
It’s absolutely essential to get all of the necessary information upfront in order to design a case correctly. Dean De Marco, chief operating officer of Succession Capital Alliance said, “During underwriting, the facts have to come out. Some advisors are reluctant to gather data from clients. But, we need this information to move the case forward. We need to tell the client what is required to underwrite a policy. We also need medical and credit underwriting. We need to understand what this loan does to the underwriting process.” Rothman said, “You need to know what to ask the client for so you are not going back and forth with them to get the necessary documents.”
Getting expert help can increase the chances of closing a case quickly and smoothly, especially for agents who are not experienced with premium financing. Delays are costly and they damage cases, Rothman added.
Experts also offered the following tips:
Managing Your Client’s Expectations
Stephan Mitchell, IUL product marketing specialist of Pacific Life warned agents not to be tempted to run a life insurance illustration at high interest rates. Run illustrations at more conservative rates to set expectations for your clients and reduce your own liability, he said.
Using Trusts to Protect the Estate
Michael L. Meyer, CPA, MBA, JD, CVA, attorney-at-law said, “Your clients want to know how to reduce taxes and you will have the opportunity to make that easier with life insurance. Taxes are not going down; they are going up. For example, there is a new Medicare tax.”
Some of the old ways of protecting an estate from taxes, like using Swiss bank accounts, are frowned upon by the IRS. But a charity package is encouraged. In fact, a charitable trust gets favorable tax treatment. Meyer suggests that when discussing a charitable trust, ask your clients how they would like it if you could cut their taxes in half? Your client will want to reduce taxes while maintaining control of their assets. That means being able to get out of the trust. At the same time, the trust has to be a good deal for the charity.
The media is rife with messy and embarrassing probate lawsuits. But a trust can protect your client’s privacy, according to Barry Engel, Esq., founding principal of Engel and Reiman. In the case of a divorce, an asset protection trust may even provide more protection than a pre-martial agreement.
Jeff Verdon, JD, LLM of Jeffery M. Verdon Law Group, LLC said that the HYCET trust can offer substantial benefits to many affluent taxpayers. Unlike with traditional gift trusts, the taxpayer and spouse can be discretionary beneficiaries, which gives them the access to the trust’s assets. A HYCET trust can be set up to defer estate taxes not just for one generation, but also for multi-generations. It should be considered for a client who wants the current $5 million gift tax exclusion, but also wants to be able to recapture some or all of the gift in case of a fiscal emergency. The HYCET trust can also protect assets from lawsuits, which is the greatest threat to an estate.
The Benefits of Forming A Captive Insurance Company
Fred Turner, founding principal of Active Captive explained that a captive is an insurance company that’s formed by a business owner to insure the risks of related or affiliated businesses. Captives come with many advantages, which explains why 50% of members of the Fortune 1500 have a captive insurance company. Benefits include the following:
• Self-insured risk: Coverage and funding for uninsured risks. Most self-insured risks can be insured through a captive insurance company.
• Reduced cost: Some coverage provided by commercial carriers may be reduced or eliminated
• Flexibility: In hard insurance markets, captives can insure unavailable or cost prohibitive risks
• Tax advantages: Captives may have ancillary income and estate tax advantages. For example, there is no tax on premium income if premiums are less than $1.2
million a year.
• Estate planning advantages: Captives give clients the ability to transfer and preserve wealth.
The ideal candidate for a captive insurance company has taxable income of at least $2 million a year, has their own company, and owns real estate.
Conclusion
As the conference wrapped up, it became clear that, whether it’s creating a trust, forming a captive, or doing premium financing, it takes a significant amount of work and preparation to meet the needs of today’s high net worth client. But getting the right assistance on the back end can help you present creative solutions that make a difference for your client and their heirs.
––––––––
Leila Morris is senior editor of California Broker Magazine and founding editor of the weekly Insurance Insider News, which she produces. She has been a business and technology editor, reporter, and writer for more than 16 years. Before coming to California Broker, she produced newsletters for life insurance agents and provided insurance industry Website content. Before that, Morris was a managing editor in charge of the successful revitalization of a telecommunications magazine. She also has extensive experience covering Capitol Hill as well as the Defense Dept. and other federal agencies. She has a B.A. in Political Science from St. Mary’s College of Md.
Voluntary Benefits – Going Green Just Got Easier for Employees
by Dominick Zenzola
Congested roads, smog, greenhouse gases these are just some of the consequences as millions of people make their way to work each day in single-occupant, gasoline-powered automobiles. To encourage employees to use mass transit and reduce the impact on the environment, employers are allowed to offer federal tax-free commuter benefits. These benefits allow employees to reduce their monthly commuting expenses for mass transit, vanpools, and work-related parking costs.
As concern about the environment has increased, other programs have been put in place. San Francisco, for instance, now mandates that employers with 20 or more employees provide transportation benefits as part of an effort by the city to reduce carbon dioxide emissions. Now, the insurance industry is taking the concept another step forward by offering optional green benefits to provide employees with an extra incentive to become more eco-friendly commuters.
Employers based in California now have the option of adding green benefits to their business travel accident policy. Standard business travel accident policies typically provide coverage for employees when they are traveling on business as well as an array of other offerings, such as kidnap and ransom benefits and identity theft services. The green daily commute, however, has not been covered under a travel accident policy. These new green benefits change that.
The first-of-its-kind coverage pays a $50,000 benefit to employees who suffer a covered injury while commuting by carpool or vanpool, mass transit, or in an alternative-fuel private passenger vehicle. All employees of California-based companies are eligible for these benefits regardless of where the employees are located. And in California, where there is already heightened concern and awareness about the environment, a significant number of people would be eligible for this insurance coverage.
Some 11.5% of commuters in California, for instance, take carpools or vanpools to work, and 5% use mass transit, according to the 2010 U.S. Census Bureau’s American Commuter Survey. Although most employees make it to work each day without incident, the commute is not without its risks. Motor vehicles are the number one cause of accidents, accounting for about 40% of all accidental deaths, according to the 2010 National Safety Council’s Injury Facts.
The cost of this additional coverage is minimal. With this new insurance coverage, employers can offer their employees an enhanced benefit package with an incentive that can be used to attract and retain employees while encouraging environmentally friendly commuting alternatives. Such incentives can be powerful tools.
For example, when offered transit commuter benefits, nearly one in five people shift from single-occupancy vehicles to public transportation, according to Commuter Benefits Work for Us, a coalition of public agencies, transit operators, private businesses and benefit providers. The impact on the environment can be significant as well. When people switch to public transportation, for instance, they can reduce their daily carbon emissions by 20 pounds, according to the coalition. In 2010, transit benefit users reduced their carbon emissions by nearly 2 billion tons. This is the equivalent to the carbon emissions from the electricity used in over 110,000 homes for one year. The savings also add up in reduced oil and gasoline use. In 2010, the use of public transportation helped conserve 52 million barrels of oil and $8.4 billion at the pump, according to the coalition.
California has long sought to combat its seemingly intractable air quality issues, and efforts to reduce emissions and traffic congestion may be starting to pay off in the Golden State. The air in Southern California is the best it has been in 13 years, according to the American Lung Association’s 13th annual State of the Air report released in April. Long criticized for their smog, Los Angeles and San Bernardino Counties have been removed from the association’s fail list for particle pollution for the first time.
In spite of these successes, Southern California still remains the smoggiest region in the nation for ozone pollution, according to the Lung Association. As the nation continues to seek ways to improve air quality and reduce smog and other damage to the environment, interest in going green has been gaining momentum.
These green benefits offer a new dimension to the benefit package that employers can provide, giving employees an extra incentive to become more eco-friendly commuters. What’s more, business travel accident policies offer other important coverages as well. Coverage options available under a global business travel accident policy include the following:
International Travel coverages
California is the nation’s number one exporting state and its proximity to Asian markets helps drive business. This means California employees may be involved in business travel abroad. A business travel accident plan provides several key coverages for employees when they travel on business outside of the United States. Emergency Medical Evacuation coverage pays for the transportation costs of an employee who is seriously ill. Political evacuation coverage pays for the cost to evacuate an employee who may be at risk as a result of political turmoil. And finally, out-of-country medical pays for medical care an employee may need in a foreign country.
Felonious Assault coverage
Employees at convenience stores and retail gas stations are not likely to travel on business internationally, but they do face risks of a different kind. Employees of these businesses often face the threat of assault and other random acts of violence. Felonious Assault coverage pays a benefit in the event an employee is injured or dies as a result of an attack on the business.
Education & Childcare coverage
If an employee dies, this coverage provides a benefit for the employee’s children to help pay for the cost of childcare and the remainder of college tuition so that the employee’s child can finish school. Although nothing can ever replace a parent, employers can help reduce the financial burden associated with an untimely death.
Additional options are also available as part of a business travel accident policy to address other risks that an employee may face while traveling. With these new green benefits, California-based employers now have another way to expand the scope of coverage for their business travel accident policies while encouraging employees to find eco-friendly ways to travel to and from work. While speaking with decision makers at a firm, agents and brokers should take the opportunity to present business travel accident coverages as well as other accident and health products and services to them. There are just too many risks not to.
–––––––––
Dominick Zenzola is a vice president of Chubb & Son and employee benefit manager for Accident & Health. For more than 50 years, Chubb has offered accident and health insurance solutions to employer groups and credit card enhancements to financial institutions. He can be reached at dzenzola@chubb.com.
