BY GREGORY O. CALLAHAN, MARC GUIEB AND DUSTIN K. POLLASTRO
Pharmacy benefit managers offer a wide range of clinical programs designed to improve health outcomes for members while reducing overall healthcare costs. Plan sponsors may find it challenging to develop a process that effectively evaluates these programs. How should plan sponsors evaluate which programs to implement, maintain, or discontinue? This article explores industry best practices plan sponsors can use to consistently assess the value of both new and existing clinical programs.
THE ROLE OF CLINICAL PROGRAMS IN PHARMACY BENEFITS
Pharmacy benefit managers (PBMs) offer numerous clinical programs focused on disease management, utilization management and medication adherence. These programs are designed to improve health outcomes through patient-focused education, provider intervention and other clinical services. One of the advantages of PBM-offered clinical programs is they are tailored specifically for a plan sponsor’s drug coverage and benefit design. This enables programs to maximize their potential clinical benefits for enrolled members through continuous, personalized care.
However, PBMs may unintentionally complicate the decision-making process as they have an interest in achieving their own internal financial targets.
Think of this common scenario: March or April comes around and your PBM account services team is ready to present last year’s plan performance review. They walk you through a PowerPoint presentation aimed at covering all aspects of plan performance using plan metrics and statistics. Within the meeting, the PBM’s account executive takes a few minutes to review a portfolio of new clinical programs aimed at plan savings and/or improved member healthcare experience.
The dilemma in this scenario is how to vet these program offerings constructively, eliminating the less meaningful programs and electing the programs with higher likelihoods of success.
A VALUE-BASED APPROACH TO EVALUATING CLINICAL PROGRAMS
The selection of clinical programs can be a difficult decision due to the complexity from a health economics perspective, especially for plan sponsors that are uncomfortable making decisions requiring expert clinical knowledge. Plan sponsors employing a pharmacy director can leverage that person’s expertise, but not all have extensive experience with clinical program evaluation. We will outline a value-based approach to assist plan sponsors in determining which programs are most meaningful to their members and what the short-term and long-term financial impacts might be.
Figure 1 is a visual tool plan sponsors can use to decide whether a prospective clinical program is appropriate for a pharmacy program. Figure 1 defines value as the relationship between effectiveness and cost.
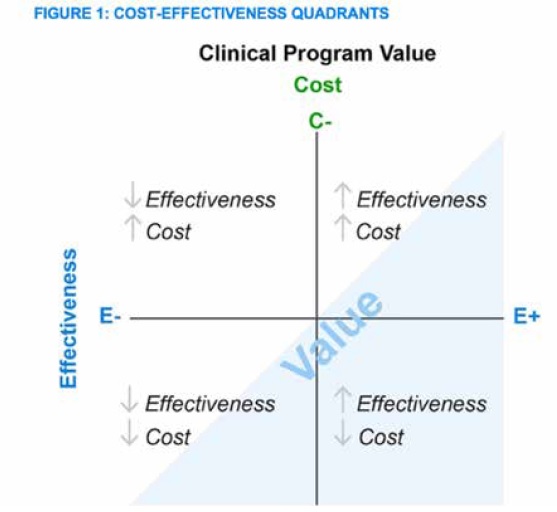
Any program that falls into the bottom right quadrant (i.e., highly effective and low-cost) should be considered, whereas programs falling into the top left quadrant (i.e., low effectiveness and high cost) should not be implemented. Programs falling in the remaining quadrants may require a more detailed analysis and the decision often depends on member demographics, culture, utilization patterns, plan design, and other individualized plan nuances.
THREE PILLARS OF VALUE-BASED DECISION-MAKING
To determine which quadrant a prospective clinical program might fall into, plan sponsors can focus on three major pillars: clinical effectiveness, financial impact, and member engagement. The first two pillars align with the axes of the coordinate plane in Figure 1 whereas member engagement is a key factor for success of the program over both dimensions. It is important to note that each pillar does not necessarily carry equal weight, that is, the relative importance of each may vary by plan sponsor.
Clinical effectiveness. Evaluate the clinical effectiveness of a program by considering which outcomes are measured and the potential of the program to achieve those outcomes.
When evaluating the outcomes being measured, it is important to identify outcomes having direct clinical significance as opposed to outcomes only functioning as surrogate markers. For example, one PBM might offer a diabetes clinical program with a measurable outcome of increasing diabetic drug adherence within one year. This metric is not ideal because, although this program can measure whether patients are filling their prescriptions, claims utilization is an oversimplified metric that does not measure:
up-front costs, ongoing fees, and potential member and/or plan sponsor savings. The up-front costs comprise both the PBM implementation fees and the costs associated with the variable full-time employee (FTE) hours increase allocated to manage the program, as plan sponsors often do not consider the extra man-hours needed to implement, run, and report program results back to their organizations. This makes the potential program savings variable and more difficult to determine, but a necessary part of properly understanding the financial impact of any value-based program.
Understanding how well the program is performing is important to evaluate performance over time and adapt when necessary.
For each clinical program, measurements for member engagement should be clearly defined and results should be presented to plan sponsors frequently, i.e., quarterly. The success of a clinical program often hinges on active monitoring and follow-up.
NEXT STEPS FOR PLAN SPONSORS
- Require PBMs to use the plan sponsor’s own utilization and data in all analyses. “Book of business” data or aggregate program results can skew projections and may not be applicable to a plan sponsor’s individual member characteristics or plan design.
- If possible, require the use of the most recent plan sponsor data to reflect the current member population. If full- year data is not available, then only the most recent quarterly data should be used and adjusted for factors like seasonality. This enables a fair comparison because outdated data can misrepresent potential program results.
- Set the expectation with the PBM account team that plan performance reviews may not be the most appropriate setting to present clinical programs. These clinical program presentations are better conducted separately from financial reviews toensure adequate time and focus is devoted toward evaluating the program.
- Require PBMs to clearly define (e.g., outline in the agreement) how patient outcomes or program outcomes are measured and, when reporting, provide the detailed calculations to support the measurements. This helps plan sponsors accurately evaluate program ROI and limits the potential for ambiguous measurements and
- Some clinical programs charge a fee per PBM Plan sponsors should require PBMs to explicitly define what classifies as an intervention. For example, an intervention could be defined as a telephone call, a 20-minute period of counseling, or another outreach method defined by the PBM.
Understanding how well the program is performing is important to evaluate performance over time and adapt when necessary. Some PBM clinical programs come with an ROI performance guarantee, so a plan sponsor must keep track of all performance year-over-year (note: understand how ROI is being calculated!)
Let’s say you decided to implement a clinical program. Fast forward three to five years—by then the conversations about the program utility or relevance have fallen out of focus and what was once a major decision has been forgotten. But the program and fees continue. How does a plan sponsor ensure the continued success of a clinical program if it is not reviewed year over year?
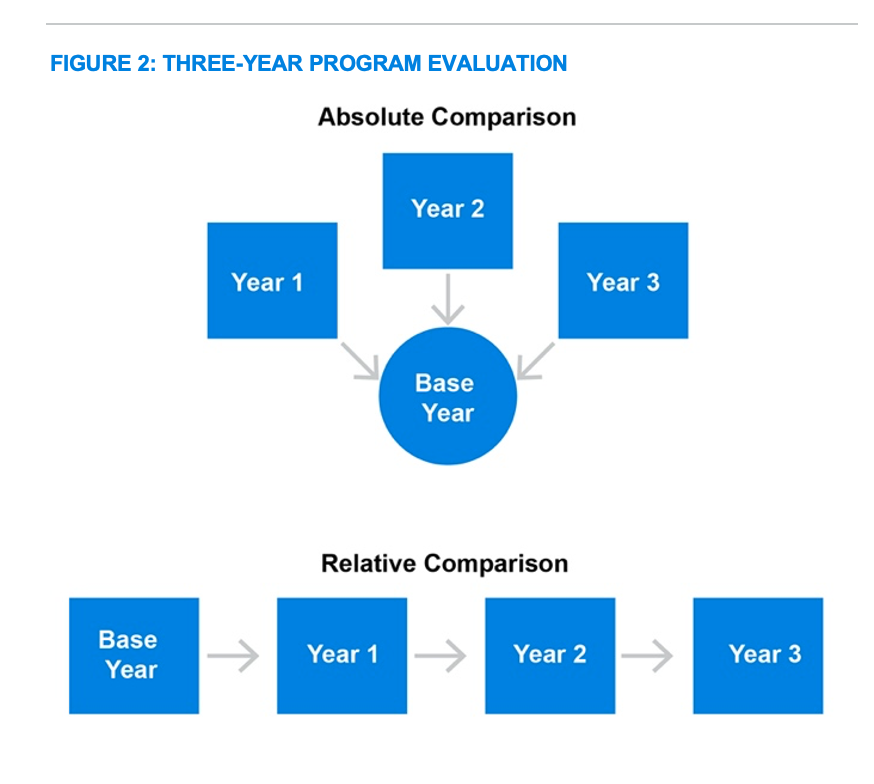
Develop a multiyear reporting plan. Always evaluate program performance in two separate measurements over time, as depicted in Figure 2. The first measurement is the absolute difference, comparing the year prior to program implementation, the base year, to each individual year that follows. The second measurement is the relative difference, comparing consecutive year-over-year differences. Using this combination of comparisons will comprehensively demonstrate how well the program is actually performing.
Understanding how well the program is performing is important to evaluate performance over time and adapt when necessary. Some PBM clinical programs come with an ROI performance guarantee, so a plan sponsor must keep track of all performance year-over-year (note: understand how ROI is being calculated!)
Finally, it is important to know when a program no longer has value and has moved to quadrant I in Figure 1 (i.e., low effectiveness, high cost). The goal of clinical programs is to achieve long-lasting effects without requiring indefinite, high-touch patient outreach. As member behaviors become ingrained habits or markets change, programs can become obsolete or less effective over time. Knowing when to turn off a program is as important as knowing when toimplement a new one. Again, continuous monitoring is essential to success, as not all clinical programs are appropriate for every plan sponsor and they can become less effective over time.
Clinical programs can be effective strategies for improving members’ health outcomes while also reducing long-term overall healthcarecosts for a plan sponsor. Plan sponsors can turn the clinical program decision-making process into a simple and productive exercise delivering value through a consistent process following best practices.
 GREGORY O. CALLAHAN, MBA
GREGORY O. CALLAHAN, MBA
Greg spends much of his time preparing and speaking at industry conferences while helping his clients manage the pharmacy/payer/PBM landscape. Greg has held high profile account management positions within the PBM industry spanning more than 13years over multiple lines of business including Managed Healthcare (Medicare), Coalition / GPO, Taft-Hartley, Commercial, Third Party Administrators, 340B, and fully insuredManaged Care Organizations. His consulting specialty is the prescription drug benefit market with experience in prescription benefit operations, PBM contracting and pharmacy program development.
 MARC GUIEB, PHARMD, RPH
MARC GUIEB, PHARMD, RPH
As a consultant for Milliman, Marc has worked in Medicaid, Medicare and commercial pharmacy benefits contracting and in claims auditing. Marc supports clients through his knowledge of pharmacy operations, regulations, formulary management, clinical trial evaluation, drug utilization review, and pipeline forecasting.

DUSTIN K. POLLASTRO, PHARMD, MBA
Dustin was a pharmacy management consultant at Milliman at the time he contributed to this article. He is now Director, Medical Outcomes Science Liaison, EMD Serono, Inc.
