BY DR. TYLER AMELL
A best practice in any employee health and benefit strategy, particularly those targeted at reducing ever increasing healthcare costs, is to collect Health Risk Assessment (HRA) information and use this data to drive your wellness or wellbeing programming strategy. Once you are able to ascertain the health status of your client’s employees, the HRA data act as a baseline to target programming on both a personal and organizational level. Further, they can measure engagement and outcomes across a wide variety of metrics as time goes on, quarter by quarter or year by year. Since most of your health status is linked to the choices you make, and the lifestyle you lead, these are the most beneficial to address from a sustainable behavior change perspective. It is all about getting people to make better decisions for themselves and their loved ones.
Examples of programming that is tied to choices and lifestyle include personalized education and training related to your health risk. Topics would include how to get more exercise for your mind and body, eating more balanced meals, drinking more water and less sugary beverages or alcohol, quitting smoking and getting better sleep. In order to be effective, personalization is critical to programming. This personalization is based upon accurate HRA information and associated behavioral data. It is not helpful if someone is a nonsmoker who exhibits good sleep hygiene and patterns ends up with programming targeted at quitting smoking and addressing sleep issues! Same for someone at a healthy weight being provided with weight loss information. It turns plan members off. Programming must speak to individual needs and interests and be tied to risk in order to yield desired outcomes.
Late last year I published an article in the American Journal of Health Promotion focused on using HRA data to help employers plan for changes in employee health that have occurred during the COVID-19 pandemic. The data revealed that brain health/mental health, including stress, anxiety and depression issues were weighing heavily on employees. Many had health indicators that were deteriorating, or not as positive as they were as we entered the pandemic. Further, preventive health behaviors such as vaccinations and screenings were negatively impacted through a wide variety of influencing factors. This meant that as we moved into future phases of the pandemic, there was some ground to make up from a health perspective. The pandemic reversed some positive momentum that many employees and employers had gained in the period leading up to 2020.
Another notable factor that was exacerbated by the pandemic was the recognition of the relationship between race, sex and gender and health disparities. There are strong relationships between these factors. However, they do not tend to be exhibited in employee health benefit data for a variety of reasons — the most important being lack of reliable data. This is where HRA data can help brokers and employers better address diverse populations in the workforce. This is due to the presence of validated and reliable questions in some National Committee for Quality Assurance (NCQA) certified HRAs. This can help employers stratify data and assure appropriate programming is meeting the needs of diverse populations.
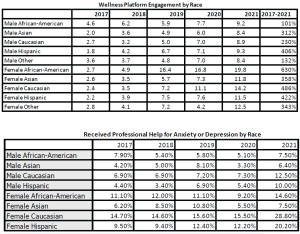
For this reason, I conducted another analysis of MediKeeper’s large HRA data set using anonymized data from Jan. 1, 2017 through Dec. 31 2021. This time, rather than limiting the analysis to sex, I included both race and gender. The results indicated that there are substantial differences in wellness platform engagement and health behaviors when you dig deeper into these data. What is revealed can have a dramatic impact on your wellness or wellbeing programming, and underlying benefit strategy. I presented these findings at the recent Art & Science of Health Promotion conference in San Diego in April 2022.
CLICK ON THE CHART TO ENLARGE
The data revealed [DTA1] widespread variation in health platform engagement, health risks and lifestyle behaviors by sex and race. Gender was not a significant factor. If these types of data are not analyzed and understood, using appropriate techniques, benefits and programming may miss the mark. In general, over the 5-year period, the racial diversity of those workers using the wellness platform increased. For example, the proportion of African American females increased from 2.1% to 8.5%, an increase of 300%. Similarly, female Asians and Hispanic representation increased 125% and 94% respectively. The proportionate decrease in female Caucasians was 19%. The same trend was seen in males, with increases of African American males of 87%, Asians of 102% and Hispanics of 44%, and a proportionate decrease in Caucasian males of 9%. The very nature of the racial makeup of the population has shifted in the time frame.
When we look at engagement as measured by unique access to the platform by race, all groupings exhibited an increase over the duration of the analysis, from a low 101% in African American males to a high of 630% in African American females. The overall average increase was 342% over 5 years. We can infer that people are increasingly interested in improving their health, or are incentivized to do so, and different races may have different motivations and may require different messaging.
In terms of exercise, female Caucasians decreased their exercise by 1.4%, while female Asians increased by 23.4%. African American females increased by 16.5% and Asian males increased by 15.8%. For those interested in exercising more, both male and female African Americans and Asians indicated a willingness to increase, while male and female Caucasian and Hispanics were interested in decreasing their level of exercise commitment.
Brain health/mental health is a key area for many employers and benefit plan sponsors, and so data by sex and race is a very useful way of assessing programing needs. Male and female Hispanics increasingly sought professional help for anxiety or depression during the study period, with a 129% and 114% increase respectively. All other races increased as well, indicating a need for these types of services, with the exception of African American males, which exhibited a decrease of 4% over the period. Perhaps outreach programming targeting these individuals will help this segment of the working population.
Similarly, stress levels increased in all races except male Asians (-10%) and female African Americans (-2%). Large increases in stress levels were seen in male African Americans and female Hispanics, a seemingly different demographic. It is apparent that different races have seen their stress levels vary during the past five years, which could be a reflection of the nature of their organizational roles.
Based on this analysis, we can safely say that if you have a racially diverse workforce, and are using a one-size fits all approach to your health strategy, it may not be reflective of the wants and needs of the population the benefit plan is designed to support.
 DR. TYLER AMELL is an internationally recognized thought leader on the topic of workplace health and productivity and Chief Health & Strategy Officer at MediKeeper. He also serves on the executive board of directors of the National Wellness Institute and the Work Wellness Institute. In the past, he served on the executive board of directors of the Integrated Benefits Institute (IBI) and the Canadian Association for Research on Work and Health. He was a past partner and vice president at a global HR consulting and technology company, CEO of a HR technology company and vice president of Canada’s largest independent health care, occupational rehabilitation, and return-to-work company. Dr. Amell holds an adjunct faculty position at Pacific Coast University for Workplace Health Sciences. He has given seminars and presentations at more than 250 events globally. Contact: tamell@medikeeper.com, Medikeeper.com
DR. TYLER AMELL is an internationally recognized thought leader on the topic of workplace health and productivity and Chief Health & Strategy Officer at MediKeeper. He also serves on the executive board of directors of the National Wellness Institute and the Work Wellness Institute. In the past, he served on the executive board of directors of the Integrated Benefits Institute (IBI) and the Canadian Association for Research on Work and Health. He was a past partner and vice president at a global HR consulting and technology company, CEO of a HR technology company and vice president of Canada’s largest independent health care, occupational rehabilitation, and return-to-work company. Dr. Amell holds an adjunct faculty position at Pacific Coast University for Workplace Health Sciences. He has given seminars and presentations at more than 250 events globally. Contact: tamell@medikeeper.com, Medikeeper.com