Six Experts Weigh In on Large Group Trends
CalBroker Magazine (CB): How has the pandemic impacted large group health in California?
Brian Sullivan, market director for Southern California, BenefitMall:
Overall, we’re starting to see the impact of the pandemic in Q4 and Q1 trends and renewals. During the pandemic, we saw many employers temporarily close their doors or severely reduce their staff, which directly impacted which group segment they qualified for, depending on the length of time the group was under duress.
While navigating the appropriate segment size, these groups also temporarily enjoyed lower premiums with higher claims, leading to higher renewal costs on their anniversaries. While there were some outliers, 2020 and 2021 renewals for the most part renewed in the single-digit area. In 2022, we are seeing the trend roll up.
“There’s a lot of interest in alternative funding solutions like level funding and administrative services only (ASO). Employers are also looking for creative wellness offerings from various carriers that provide solutions for large employers and their teammates.”
— Brian Sullivan,
market director for Southern California, BenefitMall
For a variety of reasons, the pandemic caused many people to put off diagnostics and screenings for several years. This resulted in delayed diagnoses that are more costly now than they would have been had they been detected earlier. For example, respiratory diseases moved into the #4 position over the last two years. The top two respiratory diseases are treatable through high-dollar specialty medications and gene therapy, but the cost of those meds went from tens of thousands of dollars to hundreds of thousands and even millions of dollars. Historically, $1M claims were deemed catastrophic, but over the last eight years — and more dramatically in the last two years — the new level of catastrophic claims is shifting towards $2M.
Finally, hospitals have seen significant financial losses over the last two years. Elective surgeries are their bread and butter, but elective surgeries were put on hold early in the pandemic and scheduling has not quite caught up to their pre-pandemic levels. At the same time, hospitals saw costs skyrocket as they had to adapt their practices to meet the new sterile environments that Covid-19 demanded.
Cindy Jones, SVP, Benefits Consulting department head, Dickerson Insurance Services:
Large employers are managing many moving parts post-pandemic. From managing acquisitions, to recruiting challenges, to controlling health plan costs while caring for employees, the landscape of benefit programs in this market is changing. Downsizing and right-sizing continue to be factors. As a result, employers that have traditionally been composite-rated grapple with age-rated plans as they shift to the small group market. Employee wellbeing programs are increasingly in demand. These can take the form of an expansion of existing telehealth or creative point solutions for medical and financial wellness benefits that help ease burdens for employees. Medicare expansion and exchange plan premium assistance for most income levels, while good for employee affordability, have brought about the unintended consequence of large employers struggling to meet health plan participation requirements.
“The other major trend we are seeing
among employers as we emerge from this pandemic is a focus on whole-person health, including the importance and value of behavioral health support and even specialty benefits such as vision, dental and hearing.”— Tami Adams, vice president,
Key Accounts, SoCal Sales and Account Management, UnitedHealthcare
Employee wellbeing programs are increasingly in demand. These can take the form of an expansion of existing telehealth or creative point solutions for medical and financial wellness benefits that help ease burdens for employees. Medicare expansion and exchange plan premium assistance for most income levels, while good for employee affordability, have brought about the unintended consequence of large employers struggling to meet health plan participation requirements.
Tami Adams, vice president, Key Accounts, SoCal Sales and Account Management, UnitedHealthcare:
The COVID-19 pandemic dramatically accelerated the adoption of digital health resources and benefits, including triggering a 2,500% increase in virtual care visits among UnitedHealthcare members. We are seeing that virtual care has staying power even as many people have returned to in-person appointments, with virtual care visits in 2021 among UnitedHealthcare members approximately matching the total for 2020, plus continued significant use of telehealth so far in 2022.
The evolution of virtual care is also important to its continued use post-pandemic. Virtual care has expanded from delivering care to people who are experiencing an acute medical episode to also focusing on preventing and detecting disease and helping people manage chronic conditions. Through better insights and digital tools, virtual care is also able to flag gaps in care, prevent complications, and avoid unnecessary hospitalizations — all of which can help improve health outcomes and curb costs.
The other major trend we are seeing among employers as we emerge from this pandemic is a focus on whole-person health, including the importance and value of behavioral health support and even specialty benefits such as vision, dental and hearing. As COVID-19 has further demonstrated, the body and mind are one interconnected system, so benefit programs must account for that.
Dena Allchin, director of Large Group Sales, Word & Brown General Agency:
The pandemic put a major spotlight on healthcare and the value of employee benefits. California’s largest employers were hit with astronomical challenges. They began to operate remotely — all while navigating a novel coronavirus, calculating employee and workplace safety, managing employee morale, and keeping their businesses afloat amid the many restrictions and limitations placed on commerce.
Most employers were required to shift to a remote-work environment, which brought a wave of uncertainty regarding benefits. What if employees were unable to work or telework for a certain duration of time? Could they continue benefits under their health plans, even though they were not working traditional full-time hours because of the pandemic? When should an employee be “terminated” from the policy? When does COBRA begin in these circumstances?
Employers turned to their ERISA plan documents and their health plan issuers (carriers) for guidance on these questions. Many insurance carriers allowed employees to continue benefits, even if they were (temporarily) not providing full time hours. However, most employers’ plan documents needed to be amended to allow such changes to take place. And because of the sudden timing and impact of the pandemic, many employers did not have legal resources to investigate their options for their plans. Many employers turned to their health insurance brokers for help.
The Families First Coronavirus Response Act (FFCRA) created requirements for larger employers to offer paid-time off, with benefit protection, to employees who were unable to work or telework for reasons related to COVID-19. This was a first-of-its kind mandate from the federal government, which caused a lot of initial confusion. California required employers in its state to continue FFCRA-like leave, even after the federal government made it optional for employers after the first initial several months.
“The most effective way to sell is by
providing companies with best-in-class consultative support, including benchmarks, real-time reporting capabilities, and insights into trends. Carriers need to be flexible to meet each employers’ unique needs. At the same time, benefit providers must provide a seamless, supportive, and engaging employee experience, including user-friendly digital tools and self-serve options.”Lou M. Zinzi,
head of Client Management, Group Benefits,
Guardian Life Insurance Company of America
The American Rescue Plan Act (ARPA) created COBRA subsidies, which allowed Assistance Eligible Employees (AEIs) to take advantage of premium-free federal COBRA (and Cal-COBRA in many circumstances) for a six-month window in 2021. The administration of these subsidies was complex and burdensome for employers. For this and other reasons, most employers did not see a high utilization of such subsidies.
ARPA also created enhanced Premium Tax Credit (PTC) subsidies for individual coverage applicants — capping the second lowest-cost Silver plan premiums at 8.5% of household income (extended into 2025 with the Inflation Reduction Act). While this does not impact the employer market directly, it can certainly make employees interested to know what their coverage options are in a state exchange. Employers should remind their employees that they are ineligible for PTCs on a state exchange if their employer (of any size) makes them an offer of ACA-compliant, affordable coverage.
CB: What are the most effective ways to sell to large groups in California right now? Are there particular benefits or other aspects that brokers are honing in on?
Sullivan, BenefitMall:
We’re seeing slightly different trends play out in different parts of the state. In Southern California, ACO and HMO models have really benefited employers with low monthly costs and containment in the fully-insured area. In Northern California, we’re seeing more interest in HDHP plans with incentivized and increased ER sponsorship.
There’s a lot of interest in alternative funding solutions like level funding and administrative services only (ASO). Employers are also looking for creative wellness offerings from various carriers that provide solutions for large employers and their teammates. Given that many people saw friends and family struggle during the pandemic, employers are using voluntary financial protection plans like disability, critical illness, hospital indemnity, and more to make their overall benefits offerings more attractive to prospective employees and teammates.
Jones, Dickerson:
Brokers who are looking for ways to enhance their clients’ experiences and outcomes are turning to data-driven solutions that employ analytics to focus on population health management and improve medical spend waste. On a less scientific and more subjective level, a well-designed employee benefit survey can provide valuable information about what benefits are most important to
which employee groups. Compliance remains king. Brokers who take
measures to ensure their clients are compliant with state and federal regulations are retaining clients in large numbers.
Lou M. Zinzi, head of Client Management, Group Benefits, Guardian Life Insurance Company of America:
The most effective way to sell is by providing companies with best-in-class consultative support, including benchmarks, real-time reporting capabilities, and insights into trends. Carriers need to be flexible to meet each employers’ unique needs. At the same time, benefit providers must provide a seamless, supportive, and engaging employee experience, including user-friendly digital tools and self-serve options.
As for particular benefits, an important trend is the focus on mental wellness. A recent Guardian study (www.guardianlife.com/reports/mind-body-wallet) reports that 79% of organizations say that improving the health and wellness of their employees is extremely or very important. The need is clear, as each year, one in five adults in the U.S. (50 million people) are affected by a mental health condition. Through our partnership with Spring Health, we are pleased to offer our customers access to mental health professionals and a wide range of solutions clinically proven to reduce recovery times and also help companies decrease employee turnover and increase productivity.
Adams, UnitedHealthcare:
As employers look to develop and refine health benefit plans, it will be important for our broker partners to help clients focus on integrating pharmacy, medical and specialty benefits to help support a whole-person approach to care.
We believe the future of healthcare resonates around offering choice and seamlessly connecting members to affordable healthcare. Ensuring members have accessibility to care in the right place, at the right time and for the right cost will always be a critical element of our value proposition at UnitedHealthcare.
We recognize that our partner-brokers work hard to develop coverage packages for their employers that specifically meet our members where they are in their healthcare journey. It’s an important goal we must work together to attain while concentrating on continuing to offer sustainable, affordable healthcare options to employers. Innovative solutions to mainstream barriers is key. For instance, come Jan. 1, 2023, UnitedHealthcare will eliminate out-of-pocket costs in standard fully insured group plans for certain preferred prescription drugs, including insulin and several drugs used to treat emergencies such as severe allergic reactions, hypoglycemia, opioid overdoses, and acute asthma attacks.
Eliminating out-of-pocket expenses for these critical medications can help reduce the burden of medical costs on consumers and encourage better medication adherence, reducing the risk of complications and expensive hospitalizations. And, it’s part of our company’s ongoing efforts to ensure people get the drugs they need while making healthcare more affordable. High prices are a significant barrier to prescription drugs for many people, so we are doing what we can to make a difference.
Health insurance brokers should ensure they are providing
both strategies and solutions for their large clients. Brokers are evaluating market trends and plan-utilization behavior to ensure products and plan offerings align with the needs of their clients — and their employees.Dena Allchin,
director of Large Group Sales,
Word & Brown General Agency
Allchin, Word & Brown:
Large group renewals are issued 120 days in advance, which allow employers ample time to prepare. But the large group quoting and renewals process can take some time — so it is important for the employer to begin looking at its renewal as soon as it is received.
Health insurance brokers should ensure they are providing both strategies and solutions for their large clients. Brokers are evaluating market trends and plan-utilization behavior to ensure products and plan offerings align with the needs of their clients — and their employees.
Offering a complete benefit product portfolio gives large employers access to the most health plan options for their employees. Large employers understand the importance of a strong benefits package, which helps them attract and retain talented employees.
CB: How is self-insurance or direct contracting impacting large group now?
Allchin, Word & Brown:
Self-funded insurance plans are often a strong fit for the largest employers — and are sometimes a fit for smaller employers with less than 500 FTE.
Self-funded plans allow the employer flexibility in plan design, but also create an administrative burden for the employer. In essence, the employer creates its own health plan — and the employer is responsible for full compliance with all applicable laws. Self-funded plans are subject to federal ERISA law first, then California state law.
Fully-insured plans are subject to California state law first, then federal ERISA law. The compliance items for these two types of plans are similar, but different. Employers usually have hefty compliance responsibilities when creating and administering self-funded plans.Not every employer is a good fit for self-funding, but it is worth exploring for an employer with favorable demographics.
Sullivan, BenefitMall:
The introduction of level funding has really played an important role by providing a stepping stone to employers who want more transparency and greater control over where their money is going, but aren’t quite ready for self-insurance.
Many groups that start down the road of level funding will stay in that space for three to five years. This gives them time to determine if an ASO makes sense as the next step, or if — for a variety of reasons — they need to step back to fully-insured. In Southern California, the HMO/ACO/Limited HMO options have made it particularly challenging to adapt to alternative funding arrangements.
Self-insurance combines the best of administrative, actuarial and plan development services into a program that is highly customized, customer-centric and tax advantaged for the employer.
It can also include the use of reference-based pricing, level-funding, and benefit captives.Cindy Jones,
SVP, Benefits Consulting department head,
Dickerson Insurance Services
Jones, Dickerson:
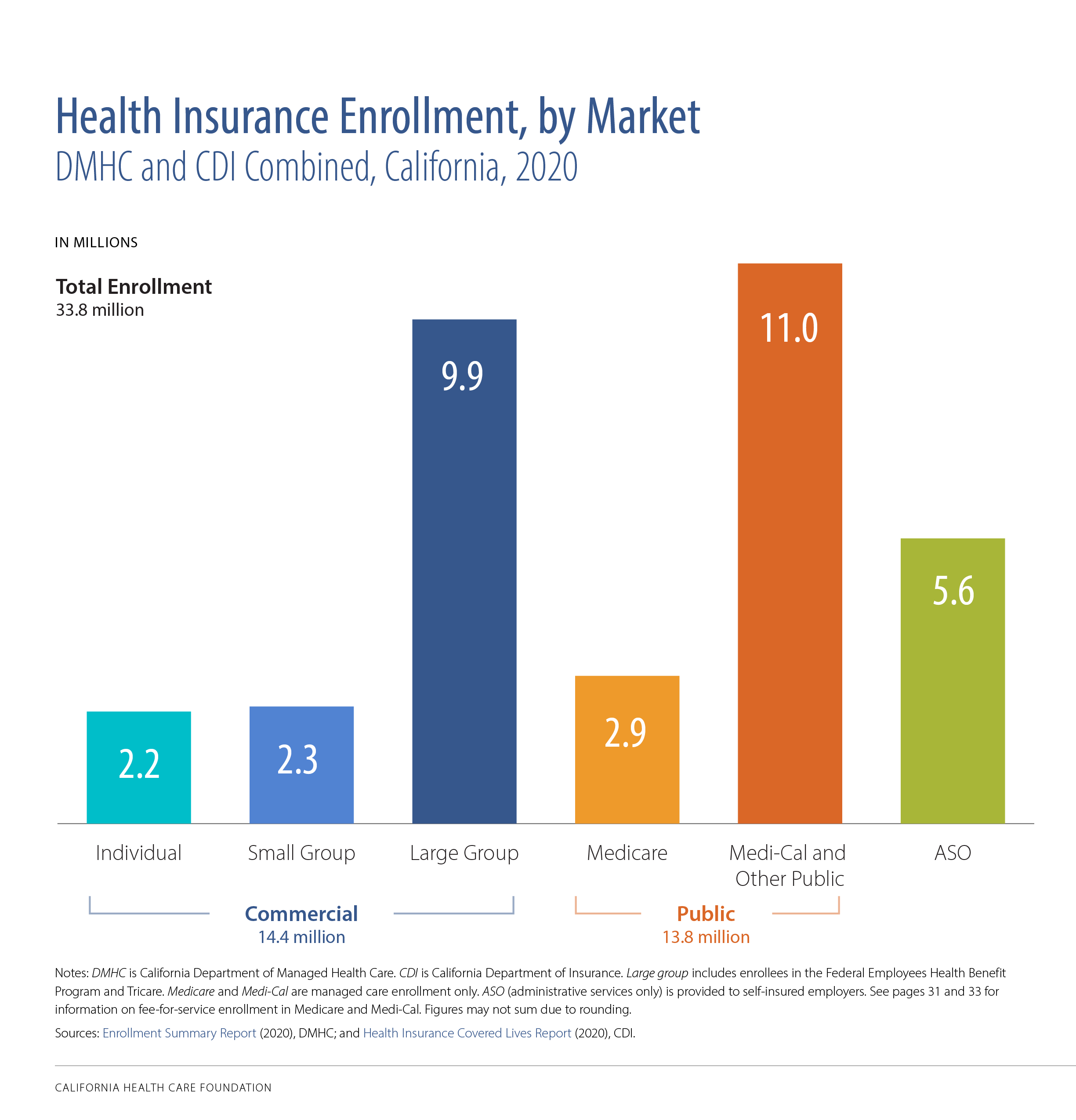
The U.S. Department of Health and Human Services reports that more than 80% of employers with 500 or more employees self-insure their benefits. A growing number of employers are taking a vested interest in how benefits are funded and how much those benefits cost them and their employees.
Self-insurance combines the best of administrative, actuarial and plan development services into a program that is highly customized, customer-centric and tax advantaged for the employer. It can also include the use of reference-based pricing, level-funding, and benefit captives. Like all other benefit programs, employee education that is delivered via a variety of media is key to the success of a self-funded model.
Direct contracting, which was the basis for many early health plans (Kaiser and Blue Cross Blue Shield), continues to be reserved for the very large and government- or union-based programs (think CalPERS).
Adams, UnitedHealthcare:
At UHC, we are seeing an increased number of clients who want more flexibility within their business model, but are still unsure about taking on the financial risks of becoming self-insured. So, what we are currently working on with an increased number of clients is the proper glidepath to support the movement to self-insured by assisting with a bridge by leveraging alternative funding.
One example is UnitedHealthcare’s Level Funding program, a self-funded medical plan designed to compete in a fully insured market like California. It mitigates the risks associated with the more widely understood self-funded models, offers fixed costs which include administration costs and stop loss premiums, limiting risk on individual claims and the group’s total claims.
It offers transparency with detailed reporting and the employer may receive a potential surplus when medical claims are less than maximum claims liability. This is designed to deliver more value for our clients, plan participants and their covered family members. Clients may even save on medical plan costs by bundling our Level Funded medical plan with UnitedHealthcare dental, vision and financial protection plans, maintaining that all important focus on whole-person health.
Not every employer is a good fit for self-funding, but it is worth exploring for an employer with favorable demographics.
CB: Is there anything on the horizon legislatively with large group health that concerns you?
Misty Baker, Director of Compliance and Government Affairs, BenefitMall:
One item to watch is AB 570 — also known as the “Parent Healthcare Act”— that becomes effective for individual healthcare coverage issued, or renewed beginning Jan. 1, 2023. This change in the law will allow adult children to add their parents or stepparents to their individual health insurance coverage. It’s possible that this will roll up to large group, but at this point, we just don’t know.
Federally, all size groups have much to plan for in 2023. Self-funded/level funded groups need to prepare for all the aspects of the Consolidated Appropriations Act, 2021 (CAA) — machine readable files, prescription drugs and many other CAA regulations will all need to be addressed.
Transparency will be a recurring theme in 2023. The CAA requires group health plans and health insurers to submit information each year to the U.S. Departments of the Treasury, Labor, and Health & Human Services regarding drug costs. Fully insured groups won’t dodge transparency requirements; they too will need to get into compliance.
Jones, Dickerson:
The 2023 ACA affordability threshold is decreasing to 9.12% from 9.61% in 2022. This, coupled with the Inflation Reduction Act that has enhanced premium tax credits for exchange plans through 2025, will continue to have an effect on employer-sponsored health plans and a large employer’s ability to meet insurance company participation guidelines. Large employers will need to be mindful of these changes as they establish premium and contribution levels for their plans.
The Consolidated Appropriations Act (CAA) Pharmacy Transparency initial reporting is due for all fully insured and self-insured plans December 2022, with subsequent reporting due June 1 of each year for the prior year. Employers of all sizes should be prepared to assist their carriers, PBMs and TPAs in completing this reporting that includes both pharmacy and general health plan utilization data points.
Allchin, Word & Brown:
For the first time since the inception of the ACA’s Employer Mandate, the Affordability Percentage for Applicable Large Employers (ALEs) has dropped below the 9.5% threshold. It is 9.12% for plan years beginning in 2023, which was a reduction of 0.49% from 9.61% for plan years effective in 2022. While not necessarily a concern, it’s important to highlight that ALEs will have to carefully evaluate health plan affordability in 2023 — with a potential requirement to increase employer contributions, in order to satisfy affordability under ACA’s employer mandate in 2023.
Fixing the “Family Glitch” is a hot item for large employers. Currently, ACA affordability is based on the lowest-cost ACA-compliant health plan at the employee-only rate. An employee who has been made an affordable offer of coverage under such standards is not eligible for a PTC for himself/herself — and neither is his/her entire family (as applicable). This can be problematic for dependents, when the ALE is not contributing much (or is contributing a very small amount) toward dependent premiums.
The Biden Administration is looking to close the Family Glitch gap under some recent proposals — however the proposed “fix” may require employers to report more information regarding their health plans to the IRS and state exchanges than ever before.
The other major trend we are seeing among employers as we emerge from this pandemic is a focus on whole-person health, including the importance and value of behavioral health support and even specialty benefits such as vision, dental and hearing. As COVID-19 has further demonstrated, the body and mind are one interconnected system, so benefit programs must account for that.
ACA IRS reporting is always a challenge for employers. There is a strong industry push via NAHU/NABIP for S. 3673/H.R. 7774 — “Commonsense Reporting Act of 2021.” If enacted, ALEs would be permitted to proactively report coverage offers to the IRS before the plan year begins (at their discretion), rather than after the conclusion of the plan year. Doing so would allow employees better up-front clarity regarding their eligibilities for PTCs and would ease annual reporting burdens during the first quarter, when employers are also completing IRS W-2 Forms.
MEET THE LARGE GROUP SURVEY PARTICIPANTS
Thanks to all our collaborative partners for sharing your trusted advice and expertise.