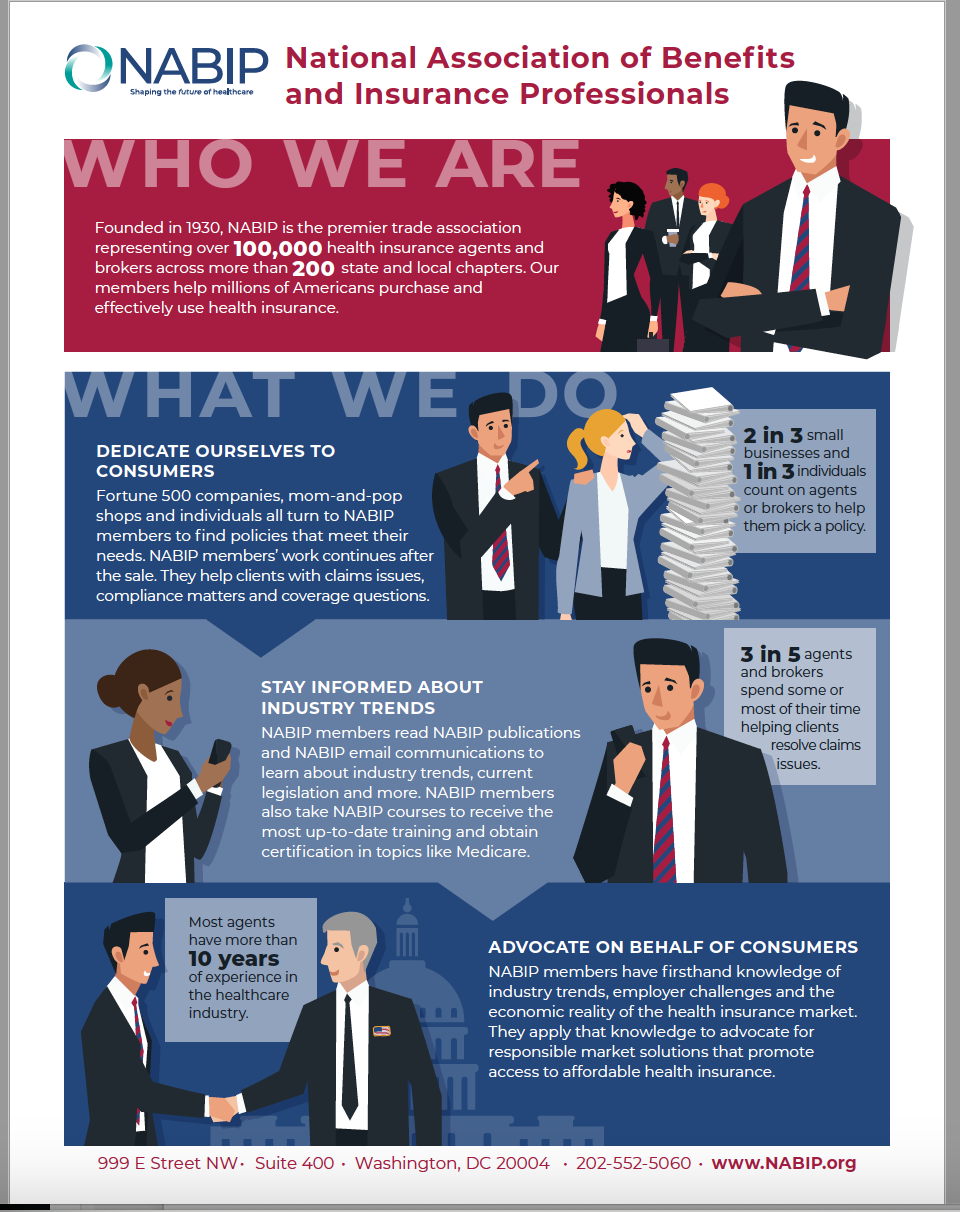
Shaping the Future of Healthcare
BY MAGGIE STEDT
Representing our association, agents and our clients, members from over 200 chapters of the National Association of Benefits and Insurance Professions (NABIP) that was formally known as NAHU, visited with their elected representatives from Feb. 26 through March 1 in Washington D.C. Chapter representatives flew in from all over the country for leadership training, to discuss key legislative issues and hear outstanding speakers. And, they visited the many DC sites, enjoyed great meals with friends and shared ideas. Members celebrated the 80’s with our NABIP Political Action Committee (PAC) fundraiser that helped raise monies for our PAC.
Members meeting with their respective congressional representatives and senators discussed the role of the insurance agent and shared following talking points that addressed a variety of issues and concerns:
Association Name Change:
- “For nearly a century, the National Association of Benefits and Insurance Professionals (NABIP), formerly NAHU, has advocated on behalf of benefits and insurance professionals. The health insurance and benefits landscape has evolved, and so has NABIP’s role in supporting our members and their clients. Over the years, our membership has grown to encompass professionals who sell traditional health insurance products and those who offer non-traditional coverage options. The association has expanded its capabilities to respond to new marketplace dynamics, offering its members a growing selection of professional-educational opportunities, network-building conferences and business-development tools.
- NABIP and our new tagline, “Shaping the Future of Healthcare” protect the association’s legacy of leadership while representing our current role in the modern healthcare industry.
While our name has changed, our mission and vision remain the same:
We believe that all Americans should be empowered to make wise healthcare and benefits decisions and have access to high-quality, affordable healthcare and related services.
Addressing the Cost of Care
- NABIP supports site-neutral rules to deter location-based gaming of coverage. One of the single most important things Congress could do is ensure that the cost of a service does not vary based on the site where it is delivered. The price of the same X-ray, MRI or physician’s visit should not differ if it is delivered in a free-standing facility versus an outpatient hospital setting.
Preserving and Strengthening Employer-Sponsored Health Coverage
- NABIP strongly opposes capping or modifying the individual tax exclusion of employment-based coverage. For decades, employees and employers have benefited from the preferences in the Tax Code that exclude the employer’s contribution toward employment-based health coverage from being considered compensation for tax purposes, allow for the pre-tax payment of an employee’s premiums for employment-based health coverage, and enable employers to deduct the cost of health coverage as a business expense. A cap on the exclusion does not address rising medical costs or limit utilization of medical services, and will stifle private-sector innovation of benefits and delivery designs. To tamper with the current tax treatment of employer-sponsored coverage would be especially devastating to businesses and American workers, which could lead to the highest increase in taxes to middle-class Americans in decades
The Commonsense Reporting Act
This act enables employers to report employer-sponsored health plan information to the IRS prospectively, before annual fall open-enrollment season in the state and federal exchanges — instead of 14 months after that open enrollment period and an entire coverage year has ended.
The bill:
- equips consumers and exchanges with information to determine if an individual is eligible for a tax credit based on their employer’s offer of coverage
- reduces the likelihood that an individual will have to pay back a premium tax credit incorrectly received
- protects employers from having to incur additional accounting and legal costs and business worries, on top of the requirement’s compliance costs, to appeal an IRS Letter 226-J tax penalty notice
- uses the current IRS IT reporting system and Exchange Data Hub, thus does not require additional federal resources
- provides employers with two compliance choices: prospectively report streamlined information authorized under the Commonsense Reporting Act OR continue to utilize the current end-of-calendar-year reporting process.
NABIP supports initiatives to innovate HSA-eligible plans.
We support the modernization of the definition of an HSA-qualified high-deductible health plan (HDHP) to allow primary care visits before application of the plan deductible. HSAs were created nearly 20 years ago, but regulations that define a qualified high-deductible health plan that can be used with an HSA have not kept pace in today’s changing benefits landscape.
NABIP opposes cost-shifting alternatives to end stage renal disease coverage.
There have been efforts in Congress to shift the cost of coverage for end stage renal disease (ESRD) from Medicare Secondary Payer (MSP) to employer plans. MSP covers ESRD for individuals entitled to Medicare based on ESRD for a coordination period of 30 months. Proposals to limit this timeframe and shift the cost to employers would create an unnecessary coverage mandate for the care of a specific disease, which could lead to an expansion of mandates for employers beyond what is already required for qualified health plans (QHPs), further driving up the cost of care.
NABIP opposes civil monetary penalties on employers for network requirements.
NABIP supports the need for adequate mental health networks. However, efforts to penalize employers for noncompliance with network-adequacy standards for mental health parity aim to penalize an entity with no control over the network. Employers use networks from carriers or third-party administrators (TPAs) and do not have control over the contracted network. Therefore, we oppose any proposals that would penalize employers for noncompliance with these standards. Instead, Congress should focus on ways to encourage mental health providers to enter into networks, which would truly support network adequacy.
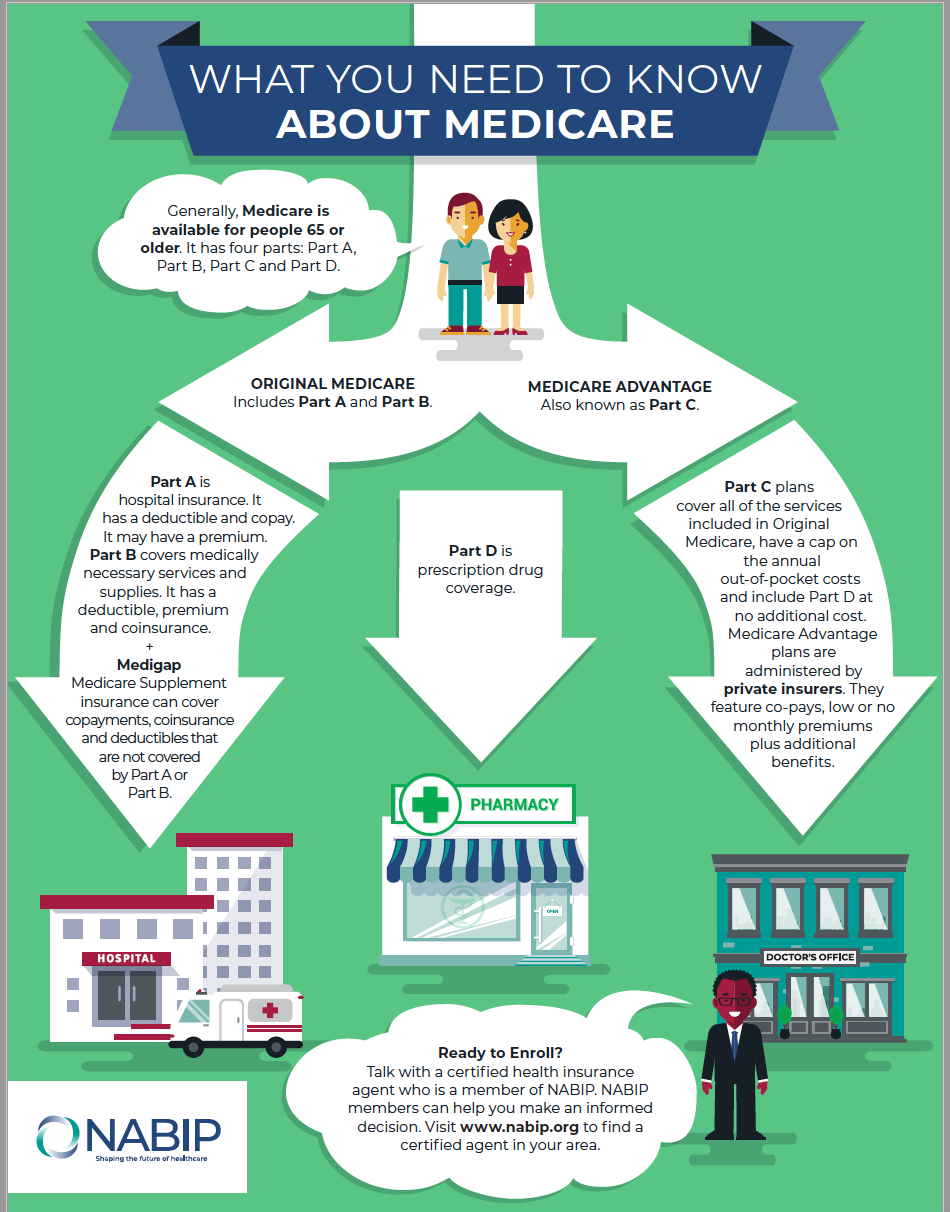
Improving Medicare
NABIP supports excluding licensed agents and brokers from burdensome marketing restrictions.
NABIP supports legislation to explicitly exclude independent agents and brokers from the current requirement to record calls with beneficiaries, in addition to any future regulations that relate to recording calls with beneficiaries. NABIP recognizes the increase in unscrupulous actors in the Medicare market; however, the CMS regulations released last year do not adequately address these entities and inappropriately target licensed and certified agents and brokers committed to acting in the best interest of Medicare beneficiaries.
NABIP supports allowing COBRA to be treated as creditable coverage.
Seniors who are enrolled in COBRA coverage but are eligible for Medicare face financial penalties for not enrolling within the mandated timeframe. However, seniors who are enrolled in similar employer-sponsored plans are not penalized, as their coverage is considered creditable for Medicare. Switching from a COBRA plan to Medicare could be disruptive for beneficiaries’ care and may come with financial consequences for terminating their COBRA coverage early to meet the Medicare enrollment windows. Seniors should be able to remain on their COBRA coverage without penalty, the same as seniors who remain on similar employer-sponsored coverage. We urge Congress to support forthcoming legislation that would allow seniors enrolled in COBRA coverage to transition to Medicare Part B without a penalty.
NABIP supports observation status to be treated as inpatient status.
Many Medicare beneficiaries are classified as being on “observation,” which can result in significantly higher claims and prevent Medicare coverage from being applied for nursing home care for patients who do not have a three-day inpatient hospital stay. We urge Congress to support legislation that would allow observation stays to be counted toward the three-day mandatory inpatient stay for Medicare coverage of a skilled nursing facility (SNF).
NABIP supports a new Part D open-enrollment period.
Many Medicare beneficiaries enroll in their plan during the Annual Enrollment Period (AEP) and are locked into their Part D coverage. Once the plan year begins, however, they are no longer able to switch to another plan if they discover they are not in the right plan for their needs. Medicare Advantage offers a three-month open-enrolment period (OEP) at the beginning of every year to allow beneficiaries to switch between plans if needed. We urge Congress to enact similar consumer protections during the OEP for Part D plans to allow beneficiaries to access the plans that best fit their prescription drug needs.”
For more information, please contact the NABIP Government Relations Team at legislative@nabip.org

MAGGIE STEDT C.S.A, LPRT is an independent contractor/licensed agent and consultant. She is a certified senior advisor and lifetime member of NAHU’s Leading Producers Roundtable at the Soaring Eagle Level. She has over 40 years of experience in essential areas of the insurance industry including sales and sales management, product development and product management. A dedicated leader, Maggie currently serves on the NAHU Medicare Advisory Committee. Founder of the annual Senior Medicare Summit, attendance grew from 200 in 2010 to close to 1,000 attendees in 2022. She served as past president of CAHIP; NAHU Region 8 Membership Chair 2014 – 2018 and past president of OCAHU, serving two terms.
Contact:
maggiestedt@gmail.com
