 Conference Features Health Reform Updates and Predictions
Conference Features Health Reform Updates and Predictions
by Leila Morris • Speakers at CAHU’s Health Care Summit, in late October, gave their take on
what to expect as healthcare reform takes shape
Today’s Business Climate Opens the Door to Retirement Plans Funded by Annuities
by Ernie Guerriero, CLU, ChFC, CEBS, CPCU, CPC, CMS • As you close your 2010 book of business, the coming year is already shaping up to be an optimal time to escort your small business clientele back to their futures and open their eyes to some new thinking about saving for retirement.
Shifting From Enrollment to Education: Now is the Time to Explain Value of Vision to Employees
by Andrea Nichelson • Enrollment season may be wrapping up, but you still have a lot of work to do if you want to help your HR clients maximize the benefits they selected for their workforce. Now is the time for brokers to arm HR managers with resources to educate employees on the value behind their 2011 benefit package.
Critical Illness Benefits Have Never Been More Relevant
by Leila Morris • Critical illness insurance isn’t a highly visible employee benefit offering because there’s still a considerable lack of awareness about the product.
Improving Medical and Fiscal Health Through Outcomes-Based Contracting
by Cyndy Nayer • Given the new push to wellness and prevention, the time is ripe for brokers to present innovative approaches to health management.
Health Reform and Dental Plans
by Mark Roberts • Now that the new healthcare legislation is the law of the land, healthcare companies and businesses are scrambling to make sense of the thousands of pages that make up the bill. One major consideration for people to decipher is about dental care.
The Future of Life Settlements
by Clark Hogan • Depending on whom you talk to, the life settlement is a superior alternative for seniors who are considering lapsing their insurance policy or it’s seen as the bane of insurance carriers and it’s rife with scams, involving nefarious individuals, smoke and mirrors, and Ponzi schemes.
Health Reform Prompts Employers To Get Creative With Wellness
by Dr. Ann D. Clark • The healthcare debate raised plenty of onfusion, but one thing that people across both aisles seemed to agree on was the need for a renewed focus on wellness and prevention at the workplace, in schools and at home.
Voluntary Benefits Volley–Our Annual Survey
Spiking Crucial Information to Brokers
This is our second annual survey of voluntary benefit plans. The strong participation of carriers reflects how popular voluntary benefits are becoming
by Leila Morris
Health Reform Prompts Employers To Get Creative With Wellness
by Dr. Ann D. Clark • The epic debate on healthcare has raised plenty of controversy and confusion, but one thing that people across both aisles seemed to agree on is
the need for a renewed focus on wellness and prevention at the workplace, in schools, and at home.
The Use of Virtual Counseling to Communicate Life Insurance Options
by Harry Gottlieb • As a life insurance professional, think about when you last selected a life insurance plan for yourself and how you went about doing it.
Why Your Clients Need Medical Evacuation Benefits
by Brendan Sharkey • As your clients travel the world, are they properly protected against financial exposure due to catastrophic medical events?
Medical Tourism Becomes An Accepted Alternative
by Leila Morris • The recent Medical Tourism & Global Healthcare Congress in Los Angeles attracted more than 1,200 from over 84 countries. The third annual conference was organized by the Medical Tourism Association.
Conference Features Health
Reform Updates and Predictions
by Leila Morris
Speakers at CAHU’s Health Care Summit, in late October, gave their take on what to expect as healthcare reform takes shape: Even with a Republican majority, don’t hold your breath for Congress to enact legislation that overturns the healthcare reform bill. President Obama has veto power. But the industry can have an influence in how HHS writes regulations to implement the healthcare reform law.
Janet Trautwein CEO, National Association of Health Underwriters, explained that NAHU has been very involved with the federal government and with state insurance commissioners to make sure that insurance agents remain part of the healthcare system. “We have an open door at the agencies and the White House. They want input from us… We are going to make sure that you get paid for the work you do,” she said. Trautwein said that the relationships that NAHU has built with the National Assn. of Insurance Commissioners (NAIC) have helped keep agents in the game. NAHU is offering its input on state insurance model laws.
NAHU wants to push for a transition period before carriers have to comply with medical-loss ration provisions. More importantly, NAHU is seeking to have agent commissions excluded from medical-loss ratio calculations.
But Trautwein said that she is worried about how health insurance will be purchased. “What if, in 2014, we have subsidies in the exchanges and small business just send people to the exchange…it would be a disaster…if large companies start sending people to the exchanges, there would be multiple trillions of dollars in extra costs to the government. That is a single payer system. We want a business friendly bill so business will want to keep providing coverage,” she said.
Neil Crosby vice president of Public Affairs, for CAHU described how healthcare reform would affect employers. He said that employers that want to keep their Grandfather status and stay with their existing health plan will have to accept rate increase without making changes. That scenario may only make sense for employers that want to preserve enhanced health benefits for highly compensated employees.
As Crosby described it, pursing the small business tax credit can be ideal for family businesses because the wages of the business owner and family members do not count when it comes to calculating average wages and hours. (The IRS actually explains the requirements in a very understandable manner at http://www.irs.gov/newsroom/article/0,,id=220839,00.html.)
To get a tax credit, the employer must have fewer than 25 full-time equivalent employees for the tax year; the average annual wages of its employees must be less than $50,000 for the year per full-time employee. The maximum credit is 35% of the employer’s premium expenses that count towards the credit.
A family member or household member of any of business owner or partner is not considered an employee for purposes of the credit. And “family member” is defined rather broadly. A family member is defined as a child (or descendant of a child), a sibling, stepsibling, parent (or ancestor of a parent), stepparent, a niece, nephew, aunt, uncle, son-in-law, daughter- in-law, father-in-law, mother-in-law, brother-in-law, or sister-in-law.
Crosby explained why the new long-term care program, the CLASS Act, is not very impressive. Many people see it as simply a creative way for the government to collect money from taxpayers to fund the rest of the health reform provisions. The government’s plan will provide a measly $50 to $75 daily cash benefit after a five-year vesting period. What that means is that participants would have to pay premiums for five years before they received any benefits. (Private plans only have a 90-day elimination period. Private plans also offer more flexibility as well as more benefits for lower premiums.) Under the CLASS Act, level monthly lifetime premiums are projected at $180 to $240 per month and are taken through payroll deduction. The government starts collecting money in 2011, but the program doesn’t start until 2013. Crosby recommended visiting www.healthcare.gov to get information on healthcare reform.
John Nelson, CEO of Warner Pacific, stressed the need for disease prevention in reducing healthcare costs. Seventy percent healthcare dollars go toward treating heart failure, coronary artery disease, asthma, diabetes, and depression. Diabetes consumes 35% of Medicare. In order to bring down costs, the healthcare system needs to support a movement toward using primary care doctors and nurse practitioners when specialist care is not needed. Nelson sees high healthcare costs and adverse selection as unintended consequences of healthcare reform. When public healthcare programs pay doctors so little, they shift the costs to the patients who can pay more.
Another concern is that, in 2014, carriers have to take all individual health plan applicants regardless of preexisting conditions and with no waiting period. There is a requirement for everyone to buy coverage, but the fine for not getting coverage is not big enough to compel most people to do so. The result is that people will wait until they get sick to buy coverage.
Nelson stressed that people in government are concerned about any adverse affects of the health reform law. They don’t want to see insurance companies go out of business. He noted that Washington State revised its health reform mandates after carriers stopped offering individual coverage. Nelson agrees with Trautwein that the industry can influence how the federal government implement the health reform law. “Rate increases have been unacceptable and you can’t blame D.C. for tying to fix it…they created a bill that can be modified,” he said.
Nelson questioned the impact that health exchanges will have. Exchanges already exist in Utah and residents are not breaking down the doors to join them. Utah’s exchange sold 50 cases last year. Since private carriers already offer a menu of choices for the consumer, Nelson asks, “Why go to an exchange?” He added, “You guys matter. Your business means a lot to the carriers…I am optimistic about the business.”
––––––––––
Leila Morris is editor of California Broker Magazine and Insurance Insider News, which she launched in 2007. She has several years of experience as a business and political reporter in Los Angeles and in Washington, D.C. She was an intern in the Capitol Hill office of Rep. Beverly Byron (D-Md.). She has a B.A. degree in Political Science from St. Mary’s College of Maryland. Morris served as a board member of the L.A. Chapter of the American Society of Business Publication Editors.
Annuities
Today’s Business Climate Opens the Door
to Retirement Plans Funded by Annuities
by Ernie Guerriero, CLU, ChFC, CEBS, CPCU, CPC, CMS
Is you close your 2010 book of business, the coming year is already shaping up to be an optimal time to escort your small business clientele back to their futures and open their eyes to some new thinking about saving for retirement.
You may want to start penciling in time with your clients to discuss fully insured plans — a tool that can help entrepreneurs and sole proprietors make up for time and investment principle lost during the Great Recession. And how’s this for an ice breaker: Fully insured plans substantially increase what small business owners can set aside for retirement while providing a significant tax deduction.
You couldn’t ask for better timing. California’s small business owners anticipate a rebound during 2011. A recent poll by The Guardian Small Business Research Institute shows that 52% of entrepreneurs surveyed in the Golden State expect sales to increase next year, compared to only 29% who predicted an upswing in business when polled a year ago. What’s more, 48% of California’s small businesses have plans to expand their businesses over the next 12 to 24 months, compared to 45% nationally. This increase in optimism means that your business owner clients may be less preoccupied with keeping their heads above water in 2011 and more willing to contemplate longer-term subjects like retirement. Fully insured plans can be a great fit for many business owners who are approaching retirement. At their core, these defined benefit pensions provide the stability of a pre-determined, guaranteed income – up to $195,000 a year in retirement benefits. Enrollees see their savings accrue on a tax-deferred basis. Once they retire, benefits can be paid out in monthly installments or in a lump sum. Company contributions are tax deductible – employees pay taxes once they start receiving plan benefits. Fully insured plans stand out in a retirement plan marketplace crowded by IRAs, 401(k)s, profit sharing and cash balance plans for several reasons:
One – They Provide a Guaranteed Return
We’ve all experienced the downside risk inherent to financial markets. The lessons of 2008 and its aftermath have taught investors, across the risk spectrum, to appreciate steady, secure returns. Fully insured plans are required by law to invest in guaranteed contracts, such as fixed annuities or a combination of annuity and whole life insurance contracts. That means they are not dependent on market performance, which helps take the risk and guesswork out of retirement savings for your clients.
Two–They Can Help Accelerate a Small Business Retirement Savings Program
Fully insured plans can help small business owners put their long-deferred retirement savings plans on the fast track. Small business owners are allowed to make annual tax-deductible contributions to fully insured plans that are potentially much larger than those allowed by other retirement options – by as much as 200% or more.
That can make a big difference. A 50-year old small business owner who wants to retire at 62 could contribute a yearly maximum of close to $176,166 to a fully insured plan. The sum dwarfs the $54,500 that the business owner would be allowed to put into a combination profit sharing and 401(k) plan. It’s more than 25% larger than what the business owner would be able to kick into a traditional defined benefit pension. There’s more: If the same owner decided to fund the fully insured plan with both a fixed annuity and life insurance, the maximum allowable contribution would swell to $221,175.
Bigger contributions are especially important for your entrepreneurial clients: When it comes to retirement savings, small business owners need every break they can get. As startups, they’ve often had to postpone or limit contributions in order to convert profits into essential working capital. There’s simply no way around it when you’re trying to get off the ground and stay in the black. Fully insured plans are a great way to catch up, especially for established businesses that no longer need to channel excess profits into office equipment, supplies, or other essential outlays.
Three – They’re Simpler to Manage Than Other Defined Benefit Plans
The annual contributions that ensure fully insured plans are properly funded to meet their obligations calculated once when a contract is first set up. There’s no annual revision or actuarial certification. If properly managed, fully insured plans will never end up over-funded or under-funded. That makes fully insured plans far easier and more cost effective to manage than other defined benefit plans.
Make Sure It’s the Right Fit
Because of their funding commitment and higher contribution ceiling, fully insured plans make the most sense for the following types of small business owners:
•
Established, profitable businesses. The large annual contributions required to fund fully insured plans make them ideal for businesses with a track record of steady profit. Typically, businesses owners who fit this profile are 40 to 70.
•
Owners nearing retirement age. Fully insured plans make it possible to supplement or augment retirement savings very quickly. That makes them particularly attractive to older sole proprietors or owners
•
Businesses with a small number of (mostly young) employees or family-owned businesses. Employers with fully insured plans, in place, must make contributions for all eligible employees. Funding requirements are typically less for younger employees than for older workers who earn more. As a result, fully insured plans can be a good fit for sole proprietorships or professional practices, such as doctors, dentists, lawyers, architects, and independent contractors. In the case of family-owned businesses, they help owners build up retirement savings for their loved ones and close relatives.
It’s important to note two caveats. First, an employer’s funding commitment is not flexible. Second, participants cannot take out loans against their balance.
While the foundation for fully insured plan funding is built on a fixed annuity base, there is room for some flexibility in plan design. Employers can incorporate whole life insurance policies that provide participants a pre-retirement death benefit in their name. One plus is clearly the death benefit that this provides key employees. At the same time, the strategy also increases the tax deduction that a company can take for contributions. Another break: Premiums are paid in tax-deductible dollars. Finally, over time, life insurance dividends can be used to reduce premiums. That way, the minimum contributions required by a fully insured plan may decrease over time.
The Cash Balance Comparison
It may strike you that another defined benefit choice – cash balance plans – might appeal to the same target group of successful small business owners who are eager to boost their retirement savings quickly. A quick comparison shows that fully insured plans trump their cash balance rivals in the following ways:
•
Fully insured plans can allow larger initial deductions than can cash-balance plans.
•
Fully insured plan benefits are backed by the insurance company that underwrites the fixed annuity and life insurance policies that serve as funding components. However, in the case of cash-balance plans, the company sponsor is responsible for any shortfall in benefits.
•
While fully insured plan contributions are calculated when a contract is drawn up and remain fixed, cash- balance plans require considerably more maintenance in the form of yearly actuarial review and certification. That makes cash-balance plans more time consuming and potentially more costly to manage.
Due Diligence Essential
There’s one very important thing to keep in mind: Fully insured plans are long-term commitments among your clients, yourself, and the insurance carrier you select. Given what’s riding in the balance — a potentially large retirement benefit spanning a number of years — your choice of the company backing the fixed annuity and whole life policy is paramount. Don’t cut corners; put the magnifying glass to a carrier’s financial wherewithal. Pore over financial ratings released by A.M. Best and other major rating agencies that scrutinize insurers and their ability to meet obligations.
Recently, you may have heard news about IRS audits of fully insured plans; this is yet another reason to scrutinize a carrier’s experience in the fully insured market. The government has red-flagged some plans that it has ruled as tax evasive. Specifically, the IRS has targeted fully insured plans that are set up to pay excessive lump sums or are funded by life insurance policies it deems to be too large. The bottom line is this: While Uncle Sam has no qualms, whatsoever, about fully insured plans as a fine retirement savings option, it’s best to sign on with a carrier that has experience underwriting fully insured contracts and knows the regulatory landscape thoroughly. Experience pays dividends to producers as well as policyholders: Chances are that the same carrier can help you draw up sales leads or backstop your efforts with Websites, literature, and call centers answer all of your clients’ questions to regarding this specialized solution.
A Golden Age for Golden State Fully Insured Plans?
For the past three years, entrepreneurs simply haven’t had a lot of time to focus on anything but the here and now. Like their counterparts nationwide, small businesses in California have hunkered down, warily watching over cash flow in the name of staying afloat. Future considerations – and retirement savings in particular – have taken a backseat until now.
In short, 2011’s long awaited boost in optimism is a prime opportunity. Take the time to get small business employers on your prospect list to open up and talk about long-range goals. According to the Guardian Life Small Business Institute, 10% of California small business owners are looking for someone else to manage the business, compared to 5% nationally. Eleven percent are looking to sell the business, compared to 9% nationally. They’re past the worst of the recession and they are starting to think about the next phase in their business and post-business lives. Introduce them to the benefits of fully insured plans and help them make the year ahead a comeback to remember.
––––––––––
Ernie Guerriero, CLU, ChFC, CEBS, CPCU, CPC, CMS, is head of Qualified Retirement Plan Marketing for the Business Resource Center at The Guardian Life Insurance Company of America, New York, N.Y. He can be reached at ernie_guerriero@glic.com or 212-598-8063.
Shifting From Enrollment to Education:
Now is the Time to Explain Value of Vision to Employees
by Andrea Nichelson
Enrollment season may be wrapping up, but you still have a lot of work to do if you want to help your HR clients maximize the benefits they selected for their workforce. Now is the time for brokers to arm HR managers with resources to educate employees on the value behind their 2011 benefit package.
Seventy-six percent of full-time employees sign up for vision coverage, but 30% of enrolled employees don’t get a comprehensive eye exam, according to a 2010 Harris Interactive survey conducted for Transitions Optical, Inc. (see Table 1).
This lack of action is a real shame, given how much a vision benefit can offer employees and their employers. Regular eye exams can lead to proper vision correction and detect early signs of eye diseases. Eye exams can also detect some costly systemic conditions, such as diabetes. Plus, lens options can help to protect and enhance employees’ vision, which has been shown to boost productivity.
HR managers sometimes worry about how plan utilization will affect their premiums, but the payoff is more than worth the investment. Nearly half of employees who are diagnosed as pre-diabetic will take steps to avoid the disease, which means they will also avoid the staggering medical costs and productivity loss that go with it, according to
HealthySightWorkingForYou.org.
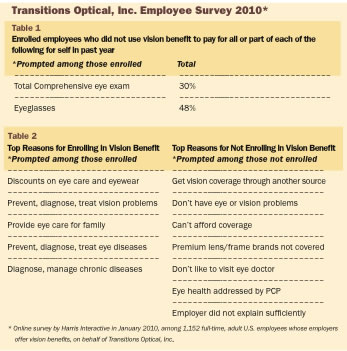
Decoding the Employee Disconnect
Why aren’t more employees taking advantage of their vision plan? Some employees may just allow their benefits selection to roll over, without giving it much thought. Others may enroll as a precaution in case they notice a vision problem or need a new pair of eyeglasses in the coming year. Some brokers might ask, “What’s wrong with these reasons?”
Many of the same reasons explain why employees sign up, but don’t use their vision benefits and why other employees don’t enroll at all. Today’s workers aren’t aware of the importance of preventative care to maintain eye health and they don’t realize how much an inexpensive vision plan can
do for them – today and in the future. Taking a closer look at the Harris survey, let’s consider some of the top reasons for non-enrollment. Let’s also explore how simple employee education from the employer – with your help, of course – can make a difference.
I Don’t Have Vision or Eye Health Problems
This is the second most popular employee response, after “I get vision coverage through another source.” It’s ironic given that going to the eye doctor is one of the best ways to keep problems from developing. An appointment with a qualified optometrist or ophthalmologist can address risk factors. A dilated eye exam can help detect many problems early on when they can often be slowed or even reversed.
Take glaucoma, which affects 4 million Americans and slowly robs victims of their side vision. Permanent vision loss can occur before it’s even noticed because people often compensate for gradual vision loss by turning their heads. In fact, half of those with glaucoma don’t realize they have the disease. It’s important for employees to see their eye doctor regularly so they can start treatment early and avoid or slow vision loss.
Also, many employees who think they are seeing well may not be. For instance, many employees learn that their persistent headaches have been caused by an out-of-date eyeglass prescription. This is significant for employers since mis-corrected vision can reduce productivity up to 20%, even when it’s so slight that the employee doesn’t even notice it, according to Optometry, 2004.
I Can’t Afford It
Even employee-paid vision benefits are generally inexpensive, with costs holding pretty steady year to year, paling in comparison with rising medical premiums. Employee contributions usually pay for themselves, especially if employees have an eyeglass prescription. Plus, quality vision plans often provide discounts on lens upgrades, provide an additional pair of eyeglasses, or supply of contact lenses, saving employees more money and encouraging them to investigate and purchase the eyewear that helps them see their best.
The real question for employees is, “Can you afford not to enroll in or use your vision plan?” Consumers value their vision. In fact, blindness is their second most feared affliction, after cancer. It’s hard to put a price on losing one of our most critical senses.
My Vision Plan Doesn’t Cover Premium Lenses or Frames
Advise your HR clients to listen carefully if employees are complaining about eyewear options not being covered. Several lens options could help employees see better and more comfortably, both at work and off the job.
For instance, photochromic lenses darken outdoors, protect the eyes from damaging ultraviolet radiation, and minimize eyestrain and fatigue. Anti- reflective coatings also minimize glare and reflections and offer cosmetic appeal. Impact-resistant materials can help protect the eyes from trauma, especially in active work environments. Many vision plan providers offer packages that cover these products including leading brands. In addition, these packages often offer a wider selection of frames that are popular with employees.
I Don’t Like to Go to the Eye Doctor
Many employees have fears about visiting a doctor, but they might not if they realize that a regular eye care checkup doesn’t have to be stressful. Vision and eye health exams are generally painless and non-invasive. Also, they can provide detection and treatment of problems that could turn into more traumatic and costly issues if not addressed early on, such as eye disease. Eye care appointments can be stepping-stones to more comprehensive medical care for people who are apprehensive about the healthcare system. Even employees who are putting off getting that inevitable pair of glasses are more likely to accept eye care as part of their overall health routine once they see how much of a difference that crisp, clear vision can make.
My General Doctor Can Address My Eye and Vision Health Problems
Just because eye health and overall health are connected, doesn’t mean that a general physical will be enough to evaluate healthy vision. Since eye care professionals specialize in this department, they are the only ones who can offer a comprehensive eye exam. They can look deep inside the eyes for clues to eye and general health issues. Just as most people still visit the dentist regardless of a visit to their primary health practitioner, eye care visits are an equally important supplement to general health visits.
My Employer Did Not Explain My Vision Benefit Well Enough
This one is a really big problem and such a missed opportunity. Employees are open to healthcare advice and information from their employers and they can use some help decoding the value behind their plan options. You can also point out to your clients that, while medical plans can get fairly complex and difficult to explain, vision benefits are typically more straightforward. Employers aren’t expected to spend as much time explaining a vision benefit as they do explaining a major medical plan. But, vision shouldn’t take up the last two minutes of an hour-long benefits presentation either. Employee communications should focus on plan costs and inclusions, the importance of vision care and vision wear for eye health, and how this benefit ties into overall health and wellness for the whole family.
Education, Education, Education
The enrollment period can be overwhelming for employees and HR managers alike. That’s why the educational process should occur year-round. Brokers can set themselves apart by offering clients educational resources to help them kick the year off right and maximize their vision plan throughout the year.
As a first step, encourage HR managers to survey employees who did not enroll in their vision benefit during the most recent enrollment period. They should identify top reasons for non-enrollment and what changes can be made to the vision plan in time for their next enrollment period.
To raise awareness of the vision benefit, among all employees, brokers can work with vision plan providers to supply HR managers with educational materials on various aspects of eye health. Most providers have handy educational websites and take-home materials that can help employees understand the importance of making eye care part of their health routine.
It is also worth exploring additional optical industry experts and organizations that share the mutual mission to raise awareness of eye health. Many eye doctors are looking to reach out to nearby employers to connect with potential patients. Brokers can serve as liaisons, introducing employers to experts who can provide medical expertise to support the argument for regular eye care. Some communities have local branches of organizations like the Lion’s Club or Prevent Blindness America (PBA), which can present information to employees or provide other materials. Finally, campaigns, such as SightSaved.org (through PBA) and HealthySightWorkingForYou.org, offer educational materials for employers and employees. Some of these materials can be customized with your name and logo, serving as a reminder of what you can bring to the table.
So keep in mind that vision benefit enrollment is only the beginning and that your HR customers will profit from a targeted approach to understanding non-enrollment and non-usage. Then determine the best ways to open employees’ eyes to the value behind this underdog benefit.
–––––––––
Andrea Nichelson is a technical and underwriting consultant with Hays Companies’ Employee Benefits Division. With 15 years risk management and insurance experience, she is a resource to clients’ HR teams in delivering innovative, effective, and comprehensive benefit programs.
Critical Illness Benefits Have Never Been More Relevant
by Leila Morris
Critical illness insurance isn’t a highly visible employee benefit offering because there’s still a considerable lack of awareness about the product. But, this coverage should become more of a priority for employers, brokers, and employees because of the tremendous value it can deliver when offered alongside group medical and disability income coverage, according to MetLife. The following is a summary of the major points of a MetLife white paper.
In today’s healthcare environment, critical illness insurance can help close the coverage gaps that come from high deductibles, uncovered expenses, and annual benefit maximums. Critical illness policies typically pay a lump sum benefits that can be used to help cover expenses (medical co-pays, deductibles, childcare and mortgage payments) related to illnesses, such as cancer, stroke, heart attack, major organ transplant and kidney failure. The claimant has the flexibility to use the lump sum payment in a way that makes the most financial sense for them. Critical illness insurance certainly fits in with today’s economy. Many employees are being hit with huge medical expenses just when they can least afford it. Dealing with cancer, heart attack, or stroke can reduce a family’s income by more than $12,000 in the first year alone, even if the patient has medical coverage, according to the MetLife Financial Impact of a Critical Illness study. The average financial burden associated with a critical illness is $35,500 — most of which is lost income. The largest non-medical out-of-pocket expenses include: travel, home or auto modifications, and home maintenance. The costs associated with a critical illness and the financial impact can be long-term.
Sixty percent of survey respondents who experienced a serious medical situation are still incurring out-of-pocket expenses three to five years after being diagnosed. On top of that, deductibles, co-pays, uncovered prescription drugs and other out-of-pocket costs can add up to over $6,500 for a typical family. Amid the tough economy, fewer people have the resources to cope with unforeseen expenses. Forty-six percent of full-time employees, surveyed by MetLife, have less than $5,000 in savings and 28% of full-time employees have less than $500.
Critical Illness Insurance and Today’s Healthcare Trends
The medical-tourism movement is likely to influence decisions by critical illness insurance policyholders about where (domestically or overseas) and when to seek treatment, as well as how to leverage lump sum payments to best cover both medical and non-medical costs. As more employees switch to high-deductible health plans, critical illness becomes an even more valuable option to offset out-of-pocket costs.
Workplace Sales
The workplace can be a logical point-of-sale for critical illness insurance because there are group rates and no medical underwriting or limited underwriting in some circumstances. Once employees learn about the cost of the coverage and the coverage details of critical illness insurance, they often develop an appreciation for its value. Roughly 75% of employees who don’t own critical illness insurance find the concept appealing once the product’s features have been explained. Most are even willing to pay the entire premium. Many said they’d be willing to pay up to $200 a year for critical illness insurance. A major selling point for critical illness insurance is that the lump sum benefit eliminates any need for ongoing paperwork and submission of bills and receipts. Furthermore, the benefit payment can be used at the individual’s discretion, providing maximum flexibility.
Clearing up Confusion
When it comes to critical illness insurance, employers and brokers have to deal with a serious lack of product awareness and downright confusion. Only 28% of full-time employees have heard of critical illness insurance and many confuse it with other kids of coverage. But, once employees understand critical illness insurance better, they find it somewhat or very appealing, even if it’s only offered on a voluntary basis and they pay for it themselves. There is definitely and unmet need. Just 7% of employees surveyed say they already have critical illness insurance. Employers and their broker partners have a tremendous opportunity to articulate a simple message about how critical illness insurance can fit into the employee benefit equation and why it should be a priority. One approach is to explain that having critical illness alongside medical insurance and disability income insurance can provide broader, more adequate, financial protection in the event of a critical illness. Making it as easy as possible for employees to understand the product can make them more receptive to participating.
Brokers and employers should emphasize how employees can use the lump sum benefit payments for anything they choose with maximum flexibility and less paperwork during the claims process. To increase the employees’ understanding of the benefits versus the cost, it’s helpful to provide personalized rate illustrations or sample rate illustrations. Ongoing communications can also help reinforce the employer’s commitment to the employees’ well being and strengthen employee engagement in the benefits program. Simple messaging and straightforward materials can all contribute to greater success.
While 65% of employees say that having voluntary benefits has made them feel more loyal at work, only 39% of employers are aware that these benefits were strong drivers of employee loyalty.
It’s clear that offering critical illness can help employers enhance the appeal of their benefit program, particularly if employees are facing larger deductibles, co-pays, and other out-of-pocket expenses.
––––––––––
Leila Morris is editor of California Broker Magazine. For more information, about the survey, visit www.metlife.com and click on “Voluntary Benefits” and then “Critical Illness Insurance” or contact Shannon Zebrick, MetLife – regional sales coordinator, Employee Paid Sales at 908-253-1622 or szebrick@metlife.com.
Improving Medical and Fiscal Health Through Outcomes-Based Contracting
by Cyndy Nayer
Given the new push to wellness and prevention, the time is ripe for brokers to present innovative approaches to health management. Value-based benefit design maximizes the value of every health dollar by offering incentives to employers, employees, health plans, and healthcare providers.
To develop a successful value-based benefit design, employers and health plans cannot simply cut costs or co-pays. They must be part of a collaborative program involving care management, treatment, and on-time results from healthcare providers. Outcomes-based contracting improves accountability and productivity among all stakeholders including employers, health plans, clinicians, communication companies, manufacturers of equipment and pharmaceuticals, hospital systems, and information management companies. Incentives must align to remove friction in healthcare delivery. The system should rely on clear and consistent communication of goals, barriers, and outcomes along with data that supports periodic adjustments to increase efficiency. Value-based benefit design can influence an employee’s choice of healthcare providers, appropriate treatments, and wellness initiatives – areas that have a meaningful impact in health status, productivity, and costs.
Incentive can include reduced out-of-pocket expenses for the following:
•
Prevention, wellness, and chronic care.
•
Use of defined networks/delivery sites.
•
Use of appropriate care providers, such as an urgent care center instead of the emergency room. Incentives can also include reduced or waived co-pays for the following:
•
Age/gender appropriate immunizations.
•
Participation in smoking cessation, lifestyle coaching, stress management, and condition management.
•
Pre-authorized/medically necessary service.
•
Use of provider networks and phone consults. For physicians and pharmacists, incentives include higher reimbursements based on outcomes and higher reimbursements for high value diagnostic and treatment services, such as minimally invasive procedures. Incentives are based on pre-determined, measurable outcomes, such as whether the patient takes a prescribed medication, for example. Increased compliance rates have demonstrated improved clinical outcomes and reduced medical expenditures. Incentives should also move the individual, provider, plan sponsor, and supplier toward the same expected outcomes for the following:
•
Better health: Lower health risks, better health status, and better quality healthcare.
•
Wealth: Rewards for efficiency and a reduction in inappropriate or redundant services, such as multi-imaging.
•
Better workplace performance: Improved safety and functional ability as well as reduced absenteeism.
Friction In the Health Value Supply Chain
Without a holistic approach, there is little engagement at the individual level or accountability across the system. Solving a problem in only one segment may increase friction in other segments. For example, if there are no coordinated incentives to manage patients who are not taking their medicine or consulting with their health coaches, the provider organization has to spend more time and money trying to re-direct the patient to healthy behaviors. If a cap on out-of-pocket expenses occurs before the patient can get all of the appropriate screenings, the patient loses out on needed exams or lab work. If the incentives are supposed to encourage the patient to adhere to a treatment plan, counseling must be considered to educate the patient on the importance of the treatment, the challenges, and the costs. Also, incentives, such as reimbursement strategies for physicians, clinicians, pharmacists, and wellness practitioners must be aligned. When healthcare is only focused on cost, there is no system to manage outcomes and stakeholders will focus on competing for dollars rather than improving health.
A value-based benefit design involves the four Ds:
1.
Data identifies the risk to the population and the organization.
2.
Design removes waste and reduces health risks.
3.
Delivery aligns service providers to focus on improving health, including engaging patients.
4.
Dividends are measurable and accrue as health resources are used for appropriate, accountable care.
When goals are aligned, the health value supply chain supports engagement at the individual and system level, which is the optimal use of outcomes-based contracting. Workers in an effective wellness program make changes that reduce their health risks and enhance productivity, which results in the following:
•
Less absenteeism rates and sick time.
•
Lower medical and insurance costs.
•
Higher job satisfaction, morale, and motivation.
Outcomes-based contracting relies on data to assess absenteeism, medical claims, workers’ comp claims, prescription use, demographics, health goals, and priorities at the workplace. Data, which measures the effectiveness of a wellness program, can be analyzed based on segmented needs. With outcomes-based contracting, employers can provide prevention and wellness programs that are tailored to the needs of particular segments of the workforce. For example, some employees need less direction to make healthy changes while others need more hands-on attention, such as a phone call from a health coach. Outcomes-based contracting moves the system away from commodity pricing and into measurable and meaningful outcomes. It also ensures that all stakeholders share the benefits of reducing health risks and the costs so that everyone benefits.
Outcomes-based contracting emerges when incentives are aligned to focus on the ultimate goal: improving employees’ health and helping employers develop predictable health cost trends. For brokers, outcomes-based contracting is a differentiator in the marketplace. Brokers can offer a tool that helps clients and payers move from chaotic price squeezing to informed population management. Brokers can present outcomes-based contracting as a way to improve performance and document health outcomes, such as more biometric screenings and immunizations or increased pharmaceutical compliance.
This harmonious approach among employees, health plans, and health systems benefits everyone, not just at the company level, but also at the community level. Since health is not static, factors affecting health should not be static either including measurement, intervention, and potential improvement, assessment, or payment for healthcare. Innovation must improve the system over time. New interventions and incentives must be aligned to support the engaged and accountable patient who manages their own health. The incentives must also be aligned to support economic improvement through engaged, accountable systems of care.
––––––––––
Cyndy Nayer is a founder and president and CEO of the Center for Health Value Innovation. Under her direction, the Center is dedicated to sharing the evidence of improved health and economic outcomes through value-based designs. Ms. Nayer provides education, insight and guidance to the Center’s growing membership as well as government leaders, high-profile media and other industry stakeholders. Outcomes Based ContractingTM is a trademark of the Center For Health Value Innovation For more information, e-mail cyndy@vbhealth.org or call 314-422-4385.
Health Reform and Dental Plans
by Mark Roberts
Now that the new healthcare legislation is the law of the land, healthcare companies and businesses are scrambling to make sense of the thousands of pages that make up the bill. One major consideration for people to decipher is about dental care. So far the analysis indicates that, except for children, dental benefits are largely unaffected.
Apparently, dental plans will be available through several options in the new healthcare legislation. According to Delta Dental of Iowa, although complete information is not yet available, a preliminary review offers the following points regarding some of the key provisions affecting dental plans and customers:
First, from a stand-alone dental benefit plan perspective, it appears that a great deal will stay the same, especially for companies with more than 100 employees. In the short-term, stand-alone dental benefits are not subject to most of the immediate insurance reforms enacted by the new law, such as no lifetime or annual maximums, and the extension of dependent child coverage to age 26. Many of the reforms and health benefit mandates contained in the new federal legislation target individuals and employers with 100 or fewer employees. Some of the reforms are effective immediately or within 6 months and others are effective beginning in 2014. Larger employers governed by ERISA are also subject to most of these changes.
For smaller employers, the legislation’s impact on dental begins in 2014. Individuals with existing coverage who are enrolled in a health benefit plan on the date of enactment (March 23, 2010) are grandfathered and subject to some, but not all of the insurance market reform changes. Generally speaking, smaller businesses and individuals will become subject to new benefit mandates as defined by an “essential health benefits package.” Under the mandates, groups with fewer than 100 employees will be required, among other things, to provide dental coverage for children up to age 21. Essential benefits can be purchased inside or outside a state or regionally-administered health exchange. These benefits must conform to an assortment of new market reforms including no annual or lifetime maximums, no copayments for some services, and an annual out-of-pocket maximum of $5,000 when combined with medical costs.
Details about the applicability of these market reforms to stand-alone pediatric dental plans will likely be written by the Secretary of Health and Human Services and are, as of now, unknown. Additionally, the final children’s dental benefit plan design is not yet defined. Within the exchanges, individuals and smaller employers will be allowed to purchase stand-alone pediatric dental coverage from companies in combination with essential medical benefits. Yet, clarification is needed to ensure that the same choice will be available to smaller businesses and individuals opting to purchase benefits in the private marketplace. In future years, larger employers will also have access to plans available through the exchanges.
Companies and individuals should focus on planning for dental benefits and taking advantage of the best plan designs. Although quite a lot of what will take place with the new legislation still needs to be sorted out, dental costs certainly will not be on the decrease. Using reliable companies that provide dental services is key and managing costs is paramount to receiving maximum care for minimal expense. There are very good plans now in the marketplace including both dental insurance and dental discount plans. Based on your needs, explore the value of both before deciding to choose a plan for a client’s oral health expenditures. If you are looking at a lot of work to be done, or just limited dental hygiene and dental maintenance, there are very good plans that are available to fit your budget, and there are many plans in the market place.
Also, according to World Dental, the provisions contained in the healthcare reform legislation expand access to dental care for children and families and seek to strengthen the oral health of all Americans while working to promote early and effective prevention. Among the provisions directed specifically at improving America’s oral health are the following:
•
Expanded dental coverage – A significant investment in ensuring access to public and private dental coverage for children in America.
•
Prevention – Dental disease prevention initiatives including public education, school-based sealant programs in all 50 states and research grants to improve the prevention and management of tooth decay in young children.
•
Tracking and monitoring – Resources for the Centers for Disease Control (CDC) and other federal agencies to assess American’s oral health and dental care with a special emphasis on pregnant women.
•
Workforce development – Expanded education of dental professionals and those who train and educate future dental caregivers in rural areas and among underserved populations. Grants to allow study options for new dental care providers.
•
Safety net improvements – Support for dental programs in school-based and community-based health centers.
•
Creation of a new commission to study oral healthcare workforce capacity.
•
Infrastructure improvements – Support for states to bolster their dental public health programs through leadership development, oral health data collection and interpretation, and best use of science to improve oral health.
•
Medicaid and CHIP – Expands Medicaid coverage and increases Federal government’s contribution to Medicaid in all states, extends the CHIP program for five years, and addresses payment to dentists and other healthcare professionals through the Medicaid and CHIP Access and Payment Commission.
Also, the addition of pediatric dental coverage, under health reform, acknowledges the connection of oral health to overall health. In effect, children’s dental services will be required to be offered through state health insurance exchanges. Additionally, the legislation recognizes the special value of stand-alone dental plans by allowing those seeking coverage through an exchange to purchase their children’s dental benefits separately from dental carriers that have decades of experience designing and administering dental plans.
Given a choice, most employers purchase dental insurance from a stand-alone dental carrier and many people prefer dental benefits offered by specialty carriers that focus on dental.
Allowing people to select stand-alone dental coverage ensures -transparency and is consistent with the current market, in which about 97% of dental coverage is provided through policies that are separate from medical plans, according to Delta Dental. In future years, as the new essential benefits requirements are applied outside of insurance exchanges, refinements will need to be made to ensure that stand-alone dental plans will continue to be available alongside medical plans.
Failure to make these clarifications could result in an unnecessary disruption of dental coverage for millions of families and create havoc. What does this mean for agents and brokers in the new healthcare landscape? There is still money to be made by offering dental to individual consumers, groups, small businesses, and large -employers. Brokers, agents, and employers can study various plans and compare specific strengths and weaknesses with the needs of their particular audiences in mind. A thorough review of information can afford agents, consumers, and employers the chance to ask insightful questions before making a decision. Dental is a highly utilized benefit that helps create employee loyalty. Therefore, it is important for all stakeholders to take the time necessary to review all the information at their disposal when selecting a plan.
–––––––––
Mark Roberts is a licensed life, health and accident insurance agent nationwide. He has a healthcare blog at www.yourbesthealthcare.blogspot.com. He’s also Medical Reporter for an online news service with over 110,000 subscribers at www.thecypresstimes.com and has contributed articles regularly to magazines for both medical and dental topics both in the U.S. and the U.K. You can reach Mark at markr@careington.com or 800-441=0380, x2905.
The Future of Life Settlements
by Clark Hogan
Depending on whom you talk to, the life settlement is a superior alternative for seniors who are considering lapsing their insurance policy or it’s the bane of insurance carriers and it’s rife with scams, involving nefarious individuals, smoke and mirrors, and Ponzi schemes.
The truth is that the life insurance policy settlement market is an industry struggling with its identity and its history, presenting itself as a form of alternative investment, allowing investors to diversify their portfolio, and enabling policyholders to sell their life insurance policies for significantly more than the cash-surrender value that a carrier might remit to the owner upon policy surrender.
The life settlement markets have been perceived as a viable, albeit risky investment strategy mostly for institutional investors. To overcome risk of the insured’s longevity on any single policy, large quantities of policies must be pooled into portfolios. This requires significant capital deployments to purchase and carry these policies to maturity and removes the asset class from consideration for all but the high net worth investor as well as institutional banks and hedge funds. There have been efforts bring the asset class to the common investor through securitizations and bond offerings, but these efforts have not been enormously effective. However, success stories do exist, whereupon life insurance policy portfolios and hedge funds have seen 12% to 15% returns after fees, even during these tough economic times. The industry does have unresolved issues. Some of the top concerns are whether life insurance settlements should be treated as securities. There is ongoing debate over federal versus state regulation of the trade. Additionally, headline fatigue has stressed the uninformed, with new articles published on a seemingly monthly basis about people who’ve been indicted for seeking funds from investors under the guise of “portfolio investments and outsized returns” only to fund their own outlandish costs of living.
All these negatives aside, life settlements are fundamentally perceived to be less volatile than their traditional financial market counterparts, provided the vehicle is directed by expert guidance. The life settlement market saw its inception in the late 1990s when viatical settlements became a sound option for AIDS patients and other terminally ill policyholders. Since that time, the industry has grown from under $1 billion to over $10 billion by 2007.
Based on conservative estimates, the market is expected to exceed $160 billion over the next several years. While the market did experience a decline in volume ($8 billion in face value transacted during 2009 according to -Conning research) experts are calling it an expected correction largely attributed to the recession and not to a collapse of the settlements market itself. Furthermore, life settlement investments have largely avoided the peaks and valleys of the major market indexes in 2008 and 2009, demonstrating strong, consistent performance that outperformed the S&P and most exchange traded funds.
Are They Securities?
The Government Accountability Office released a July 2010 report confirming what those in the life settlement industry already knew– life settlements deliver an average of eight times more to the policy sellers than what carriers can offer in surrender payouts. The Life Insurance Settlements Association website notes that the industry creates $7 million per day in value for seniors who opt for a life settlement. The Securities and Exchange Commission has made efforts to approve life insurance policy securitizations. The goal is to bring more protection to the investment community by placing the investment class under FINRA jurisdiction while opening the investment class to retail investors. This has largely been opposed by the ACLI, which says that there would be increased risk of fraud to create product via stranger originated life insurance policies.
Insurer Opposition
Insurers have been trying to curtail growth of the life settlements -industry. Many have implemented contract language prohibiting agents from discussing life settlement options with their clients. According to the Life Insurance Settlement Association (LISA), more than 90% of all life insurance policies lapse with no payout to the beneficiaries, which means more payouts for insurers. Actual data from 1995 to 2008 indicates that 45% of all insurance policies lapsed. During that period, a mere $38 billion, or 0.3% of life insurance policies were settled. This data refutes any distorted claims by carriers that the life settlement industry is a significant threat to the insurance industry.
Some carriers have attempted to prohibit settlements by inhibiting the brokers’ and agents’ ability to discuss the option of life settlements with clients. It puts brokers in a difficult position – comply with insurer requirements, risk losing the business, comply with state guidelines, or face possible legal action from the uninformed client. Many brokers are choosing to fulfill their fiduciary responsibilities and take their chances with the insurer community. Some states are now requiring that brokers and agents inform their clients of the option of the life settlement market.
The Federal Government Versus State Regulation
Despite insurance carrier opposition, the federal government is seriously considering the feasibility of the life settlement market. At the moment, life settlements are regulated in 40 states and Puerto Rico. The 2010 Financial Reform Law continues the current state-based regulatory system. It adds a Federal Insurance Office to oversee the insurance industry. The office is charged with evaluating state insurance law for inconsistencies and conducting a cost/benefit analysis of possible federal regulation. The law also creates the Office of Financial Protection for Older Americans, designed to locate unfair or deceptive financial advisor certifications. Life settlement industry experts point to this office as the next source of regulation and standards development for the industry.
With increasing attention from the federal government, the life settlement industry is gaining a strong foothold in the investment community. Most states are adopting life settlement regulations and banning stranger-originated life insurance (STOLI) practices (buying insurance with the intent to resell it on the life settlement market.) Brokers will be required to understand the market and advise customers on life settlements as a credible option. Also, the National Conference of Insurance Legislators (NCOIL) is supporting regulations that require insurers to inform their policyholders of all options available to them, including life settlements. A number of U.S. and European associations are joining forces to bring more transparency, consistency, and investment decision-making tools to consumers. The life settlement market welcomes the additional transparency. The industry has operated well under current conditions, but additional regulatory oversight can go a long way toward reassuring brokers and clients of the strength of their investment advice and decisions.
In 2007, NCOIL adopted its Life Settlement Model Act; the 28-page document outlines proposed rules and standard practices — from licensing requirements and disclosure to fraud prevention and penalties. LISA officials and membership approved the Act and many life settlement brokers and companies have implemented the plan.
In an environment of financial upheaval, the settlement industry continues to make significant inroads.
While the life settlements markets have indeed slowed over the past two years, they have remained vibrant, and interest is growing.
Investment returns on portfolios have increased, which suggests improved life settlement industry expertise from fund managers in understanding the underlying product. These successes will invigorate renewed investor interest as they search for consistent profits. New stress tests indicate insurance carriers are strong enough to withstand the existence of the life settlement marketplace and continued efforts on behalf of government towards regulating the industry will improve the industry and remove the bad players.
The financial advisor community can no longer ignore the potential for their clients. As standards and codes of conduct are developed and implemented, policy sellers and potential investors will be seeking expert guidance in navigating this new option.
Life insurance professionals and financial advisors alike should take a proactive approach in understanding life settlements in order to create worth for their clients. Industry organization websites, such as www.thevoiceoftheindustry.com are a great first step for those interested in learning about and connecting with accredited professionals.
––––––––––
Clark Hogan is managing director Opulen Capital. For more information, call 877-678-5361 Direct or 310-721-1655, e-mail Clark.Hogan@OpulenCapital.com, or visit www.OpulenCapital.com.
Voluntary Benefits Volley–Our Annual Survey
Spiking Crucial Information to Brokers
This is our second annual survey of voluntary benefit plans. The strong participation of carriers reflects how popular voluntary benefits are becoming
1.
Please list the voluntary/employee-paid benefits that you offer along with the minimum group size for each offering:
Aflac: Aflac’s policies, from accident/disability to vision, offer direct-to
the-policyholder cash benefits, unless otherwise assigned, to help cover what other insurance does not. Following is a list of individual plans* available through Aflac:
• Accident
• Cancer/specified-disease
• Dental
• Hospital confinement
• Hospital intensive care
• Life
• Lump sum cancer
• Lump critical illness
• Specified health event
• Short-term disability
• Sickness indemnity
• Vision
*Certain policies may not be available in all states.
The following is a list of group plans available through Aflac Group:
• Accident
• Critical illness
• Dental
• Hospital
• Life
• Short-term disability
There is no minimum participation requirement for our individual plans. We only ask that the client establish an account with us by completing and signing a Payroll Account Acknowledgement form and allowing three separate W-2 employees to enroll in at least one of our plans. Aflac Group requires a minimum of 25 payors to establish group billing.
Ameritas: Ameritas Group offers dental, eye care and hearing on a voluntary basis. Dental and eye care begin at 10 lives and hearing at 50 lives.
Cigna: CIGNA Voluntary is a division of CIGNA HealthCare, offering limited-benefit medical, dental, pharmacy and vision care plans and discount programs, as well as group life and accident disability insurance. All CIGNA voluntary products are available to groups with at least 51 eligible individuals.
Colonial Life: Colonial Life offers voluntary benefits to businesses with as few as three employees up to thousands of employees. Our product portfolio includes individual and group voluntary products for short-term disability; term, whole life and universal life; hospital confinement, cancer; critical illness; and accident.
Delta Dental: Delta Dental of California’s voluntary dental plans are for employers, associations, affinity groups, and other trust organizations that wish to offer employee-paid comprehensive dental coverage. Delta Dental offers a variety of features and benefit plan designs that allow employers to offer our Delta Dental PPO, Delta Dental Premier and/or DeltaCare USA products to meet their needs. These dental plans have the same quality standards, cost savings, and ease of use as our employer-financed products. Plans are available based on a variety of premium contribution levels from fully employee paid to some level of employer contribution. Voluntary plans require a minimum participation of five primary enrollees.
Golden West Dental & Vision: DHMO dental – minimum two enrolled.
PPO dental – minimum five enrolled and 25% participation.
Guardian: Guardian’s comprehensive employee benefits portfolio
includes the following voluntary/employee-paid benefits:
•
Dental (minimum of five enrolled).
•
Vision (minimum of five enrolled).
•
Life (minimum of 10 enrolled).
•
Short-Term Disability (minimum of 10 enrolled).
•
Long-Term Disability (minimum of 10 enrolled).
•
Accidental Death & Dismemberment (minimum of 10 enrolled).
•
Critical Illness (minimum of 10 enrolled)
Health Net: Health Net offers voluntary dental, voluntary vision, and voluntary term life coverage to groups of two or more. Voluntary term life is offered as a buy-up option to basic group term life coverage.
Humana: The minimum group size for the voluntary products is five
lives. Humana offers a comprehensive suite of products that includes: life, disability, accident, critical illness, cancer and supplemental health.
MetLife: Through various arrangements, MetLife and its affiliates offer the following voluntary/employee-paid benefits: group auto and home (employers with 500 or more employees); Underwritten by MetLife Auto & Home, a brand of Metropolitan Property and Casualty Insurance Company and its affiliates: Economy Fire & Casualty Company, Economy Preferred Insurance Company, Metropolitan Casualty Insurance Company, Metropolitan Direct Property and Casualty Insurance Company, Metropolitan General Insurance Company, Metropolitan Group Property and Casualty Insurance Company, and Metropolitan Lloyds Insurance Company of Texas, all with administrative home offices in Warwick, RI. Group Legal (employers with approximately 10 or more employees) through Hyatt Legal Plans, Cleveland, Ohio, or Metropolitan Property and Casualty Insurance Company or its affiliates, Warwick, RI. Critical Illness (employers with 500 or more employees).
Unum: Accident – 10 lives, specified critical illness — 10, Group critical
illness – 250, MedSupport — 10, term life — 10, Interest-sensitive whole life –10, universal life — 10, group voluntary short term disability — 10, voluntary individual short term disability — 10, group voluntary long term disability — 10, individual disability — three, group voluntary long term care – 15, individual long-term care — three, and AD&D — 25
2.
Do you have any benefit offerings for employees that work fewer than 40 hours a week?
Aflac: Yes. All of our individual and group plans are available to all full
time employees, as defined by your client, that work less than 40 hours per week. Please note the following:
•
Individual accident and short-term disability plans — Employees must work a minimum of 30 hours per week.
•
Group accident and short-term disability plans — Employees must work a minimum of 16 hours or more per week. Seasonal and temporary employees are not eligible for coverage under our group plans.
Ameritas: All our benefits can be reviewed and customized to accomodate work hours less than 40 per week.
Cigna: Yes. CIGNA Voluntary is a leading provider of limited-benefit
health plans for full-time and part-time hourly employees. We serve industries, such as hospitality, retail, staffing, and construction. Our plans offer a reasonably priced health insurance option for employees who don’t qualify for major medical plans. Employers who offer our plans can experience reduced turnover, improved recruiting and more predictable benefit expenses for their hourly workforce.
Colonial Life: Yes. All of our products are available to employees who work a minimum of 20 hours a week. Employees must be actively at work and a permanent employee of the employer group.
Delta Dental: Yes. The client specifies eligibility rules. Our voluntary plans are a solution to the benefit needs of part-time employees, retirees, association members and cafeteria plan participants.
Golden West Dental & Vision: Yes. We offer all our products down to 30 hours per week.
Guardian: Yes. Guardian benefits can be offered to employees that work less than 40 hours a week.
Health Net: Yes. Health Net allows coverage for full-time employees working 30 or more hours per week.
Humana: Yes. Many of our groups have associates who work 20 hours a week. We also offer solutions for various groups and classes within one employer group. Long-term care (employers with approximately 10 or more employees); Pet Insurance (employers with 500 or more employees) through National Casualty Company, Madison, WI, and veterinary pet insurance Company, Inc., Brea, Calif.; Disability (employers with approximately 10 or more employees); life (employers with approximately 10 or more employees); and vision (employers with 500 or more employees), through EyeMed Vision Care, Mason, Ohio.
MetLife: Yes, MetLife and its affiliates work with each employer to determine the eligibility requirements for the employee population. However, we also adhere to all applicable laws and regulations concerning eligibility, which, in some states, exclude those not working more than 24 or 30 hours a week.
Unum: Yes, our offerings are available to employees who work 20 hours.
3.
Do you offer flexible enrollment data, billing capabilities and processes that work with the employers’ systems instead of the other way around?
Aflac: Yes. Aflac Wingspan Enrollment Solutions help remove enrollment obstacles by streamlining the benefit enrollment process for your client and their employees. Our technology-based services can help simplify the enrollment process. We offer the following enrollment methods:
• One-on-one laptop
• Call center
• Web self-service
• A combination of the above
These services are provided to your client and their employees at no direct cost. Through our SmartApp Next Generation software, we can process a large number of policies quickly and accurately. Business submitted through our software, located on our agents’ laptop systems, can be issued without human intervention (resulting in a 24-hour turnaround time). These services apply to our individual plans only. Aflac has the capability to transmit billing data to an account in a variety of different ways. Aflac agents will work with your client to discuss available enrollment and billing options and determine which options will best meet their needs.
Ameritas: Yes, our goal is to keep the difficulties of administration behind our walls. We offer many flexible solutions that work with our customers’ systems.
Cigna: Yes. Whether an organization represents a few hundred or thousands of part-time and hourly workers across the nation, we have a solution that will reduce the burden of plan administration. We can provide files that can be uploaded to interface with a client’s own payroll system.
Colonial Life: Yes. Colonial Life’s Harmony enrollment system is built to accommodate the various needs businesses have for enrollments and data reporting. We can enroll employees face-to-face at any business location and any work shift. We can also provide employers with daily enrollment reporting, such as which employees have been seen and what they’re buying. This reporting capability allows the employer to assess the enrollment’s progress daily and make any necessary adjustments. Colonial Life also has several electronic services for businesses that allow them to receive their bill online, make payments online and make any necessary billing adjustments online.
Delta Dental: Delta Dental has extensive experience working with a wide variety of employers’ systems and third- party administrators for the purposes of eligibility, enrollment and billing. We can accept eligibility transmission in the following formats:
• Secure File Transfer Protocol (SFTP)
• FTP with PGP encryption
• E-mail with PGP encryption
• Secure e-mail monitoring system
• Secure website (Delta Dental pick up or customer drop off)
• Web enrollment/directly online
• Enrollment cards
Guardian: Yes. Guardian offers a wide range of enrollment options (electronic eligibility files, online and paper enrollment) as well as billing options (online, paper and electronic fund transfer) to meet the varied needs of employers and ensure ease of administration.
Health Net: Health Net has a variety of enrollment and billing options, including electronic eligibility data transmission and Web-based tools. The company also offers a standard format for electronic eligibility transmission. If a client has a preferred format, Health Net will accommodate employers’ preferred formats whenever possible.
Humana: Our goal is always to put the customers’ needs first. Enrollment data can be captured and transmitted via paper or most EDI files. Billing can be set up as a self bill or list bill and the client can remit payment via check or electronically online.
MetLife: Yes, MetLife, for itself, and as the billing service provider for its affiliates, is able to work with virtually all types of payroll systems.
Unum: Yes
4.
Do you offer the flexibility to conduct enrollments through one-on-one benefit sessions, group meetings, call centers, and online self-enrollments?
Aflac: Yes. We have the flexibility to conduct enrollments through each of the methods listed. However, the availability of each method is determined by the number of eligible employees.
Ameritas: Yes, Ameritas Group offers many different ways to enroll depending on the needs of the customer. All options above are involved depending on the number of lives being enrolled.
Cigna: Yes. Each client is unique; how they communicate with their employees often depends on specific worksite characteristics. Our goal is to work with our clients to determine the enrollment support that makes sense. CIGNA Voluntary clients can choose enrollment methods that best meet their needs and fit with their culture:
•
Paper enrollment forms (we can provide or the client can customize)
•
The CIGNA voluntary enrollment center (we also offer foreign-language assistance)
•
The CIGNA voluntary on-line/Web enrollment (24/7 user-friendly access)
Colonial Life: Yes. Colonial Life offers a full spectrum of benefit communication and enrollment options, including group meetings, one-to-one meetings, call centers and online self-enrollments. Our national team of local, professional benefit counselors uses the Harmony enrollment system to educate and communicate benefits to employees face-to-face so they can make better benefit decisions. For hard-to-reach employees, we can offer the same benefit communication and education experience by co-browsing with employees on the Internet, meeting through a call center or setting up online self-enrollments.
Delta Dental: For groups over 100, Delta Dental representatives are available to participate at open enrollment meetings and health fairs to provide information pertaining to our dental plans. We provide open enrollment support at no additional cost. Customized videos are also available in a variety of formats that explain the client’s specific benefit information and can be played at open enrollments or new hire orientations. Customer service is available to support questions about a plan’s coverage, but cannot accept enrollments. Enrollment is facilitated by the benefit administrator. Delta Dental provides benefit administrators with access to an application that allows enrollees to select a benefit package online during open enrollment and update their personal information online year-round.
Golden West Dental & Vision: Yes.
Guardian: Guardian offers the flexibility for employers to offer a choice of enrollment methods to employees, including online self-enrollment and paper enrollment kits that can be personalized to each employee (in English & Spanish). In addition, Guardian offers additional support services, such as group meetings conducted by a certified enrollment specialist, toll-free benefit hotline in over 50 languages and turnkey employee communications at no additional cost to ensure the enrollment process is simple and easy for both employers and their employees.
Health Net: Health Net provides on-site support, including bi-lingual representatives if needed, to assist employer groups with new case and renewal enrollment meetings. Additionally, our Customer Contact Center is available to answer any questions from current and prospective members and clients.
Humana: One of our key selling points is the ability to offer comprehensive enrollment solutions. As part of Humana’s consumerism philosophy, our goal is to educate the employees about the products and services available to them and their families. A typical enrollment scenario may include payroll stuffers, enrollment posters, email blasts, then a face-to-face enrollment with the ability to capture any other associates through our call center or online enrollment capabilities.
MetLife: Yes, MetLife and its affiliates conduct enrollments/application processes through group meetings, our call center, and online. We work with the broker and employer to determine which enrollment/application channels will provide the best experience for a particular employee population.
Unum: Yes
5. Do you honor broker-of-record letters?
Aflac: Yes.
Ameritas: Yes
Cigna: Yes.
Colonial Life: Yes.
Delta Dental: Yes.
Golden West Dental & Vision: Yes.
Guardian: Yes, Guardian honors broker-of-record letters.
Health Net: Yes.
Humana: Yes. Additionally, all of our broker contracts
are vested.
MetLife: Yes.
Unum: Broker-of-record letters apply to voluntary at a case level (while
the individual policies remain vested).
6.
Do you offer simple and hassle-free account billing and payment processes?
Aflac: Yes. Our goal is to make billing and payment of premiums simple and hassle-free for your client. Aflac’s systems are flexible enough to accommodate a variety of billing methods and handle almost any type of billing layout. Your client can be billed electronically, via paper, or your client can participate in Aflac Wingspan Online Services for accounts. Depending upon the billing method selected, your client will receive an invoice containing the premium amounts due for the policies of the employees participating in our plans. The payroll-deducted premiums, for the employees, may then be remitted to Aflac via check, wire transfer, or through an automated clearinghouse.
Ameritas: Absolutely, our goal is to take the burden off of our customers. We listen to their needs, then enhance our billing and payment processes whenever necessary to make sure we’re meeting those needs.
Cigna: Yes. We offer automated premium tracking with auto-termination functions to alleviate management of any outstanding balances and missed deductions. After our clients collect premium through payroll deductions, they can easily forward amounts to CIGNA Voluntary by check, wire or ACH.
Colonial Life: Yes. Colonial Life has several electronic services for businesses, which allow them to receive their bills online, make payments online, and make any necessary billing adjustments online. Colonial Life also offers Ez Billing to reconcile the bill for the account.
Delta Dental: Yes. Delta Dental has several billing and payment formats available depending on the client’s plan and preference. Our online billing and reconciliation application allows benefit administrators to view, pay, and reconcile enrollment online. Online features include the following:
Invoice Presentment:
•
Shows the details of a selected invoice.
•
Allows the administrator to attach a note to an invoice and submit back to Delta Dental’s Enrollment & Billing department.
•
Enables the benefit administrator to download an invoice and save it as an Excel spreadsheet.
•
Provides easy access to current and historical invoices and their associated notes
Payment:
•
Provides a convenient and secure method for invoice payments.
•
Provides option of paying invoices online or printing or mailing the remittance statement with payment.
•
Allows the benefit administrator to view and track payment history.
Group reconciliation:
•
Enables benefit administrators to submit enrollee additions, changes and terminations
•
Includes tools to automatically compare a Delta Dental invoice to client’s remittance file and view and/or download results.
•
Offers a view of the line-item adjustment summary
Golden West Dental & Vision: Yes.
Guardian: Yes. Guardian offers a range of billing and payment options
from online to paper to electronic fund transfer to help meet the varied needs of employers and ensure ease of administration.
Health Net: Yes, Health Net offers simple, hassle-free account billing
and payment processes including Web-based tools to assist our clients and their brokers.
Humana: Once a case is sold, a dedicated account installation manager will implement it. Each case will also be assigned a dedicated billing representative who will assure that the monthly bill is timely and accurate.
MetLife: Yes. A single bill file platform is available for all voluntary benefit products, which allows a single customer payment on a per pay period or monthly basis.
Unum: Yes.
7.
Does your billing system allow plan administrators to make online deletions and changes to their plan account?
Aflac: Through Wingspan Online Services for Accounts, Online Billing
allows your client to safely update, reconcile, and pay their Aflac invoice electronically. This automated service enhances accuracy, speeds transactions, and minimizes paperwork. Your client will save time and money as their electronically remitted payments and changes are processed faster.
Ameritas: Yes
Cigna: Yes.
Colonial Life: Yes. Colonial Life offers online billing capabilities. A plan administrator also has the ability to make changes, as well as update employees’ coverage and general information.
Delta Dental: Yes. Delta Dental’s online eligibility management system allows the clients’ representatives to add or terminate enrollees and dependents and modify enrollee information through a secure website. Enrollment changes made by the client using our online eligibility system are made to the system in real time.
Golden West Dental & Vision: These may be emailed to our accounting department.
Guardian: Yes. Guardian’s benefit website offers a one stop source for plan administrators to manage their account online, including submitting eligibility changes that impact their bill. Plan administrators have the flexibility to recalculate their bill online to take into account any eligibility changes so they can adjust payments accordingly.
Health Net: Yes. Plan administrators may make most enrollment changes online.
Humana: Currently, the system permits groups who have purchased group term life to make such edits, but functionality for the voluntary benefits will not be available in 2011.
MetLife: Yes. Through our online billing system per pay period deduction amounts can be changed in accordance with each payroll run.
Unum: Yes.
8.
Does your billing/payroll deduction process make it easy for the employer to offer multiple products?
Aflac: Yes. Aflac can facilitate even the most complex enrollment scenarios. Our Core Benefits Plus Aflac enrollment system allows employees to keep their current coverage with other carriers. This system enables employees to enroll for core, voluntary, and ancillary benefits on a single software platform. Our Core Benefits Plus Aflac enrollment system is developed to meet the needs of each individual client. Aflac’s Response Requirements for Core Benefits Plus Aflac:
•
100 or more eligible employees for a laptop enrollment.
•
500 or more eligible employees for a Web self-service enrollment.
•
Six weeks lead-time.
•
Minimum of three Aflac plans offered.
•
1GB RAM for laptop enrollments (may require up to 2GB RAM).
•
A customer agreement on the implementation schedule/timeline.
The number of total lives on our Core Benefits Plus Aflac system is more than 21,000.
Aflac’s largest client that utilizes our Core Benefits Plus Aflac system has 2,000 employees with a 25% to 35% penetration rate.
Ameritas: Yes. Making it easy to offer multiple plans is our expertise.
Cigna: Yes.
Colonial Life: Yes. Colonial Life can enroll an employer’s core and
voluntary benefits and provide the employer enrollment data on all employee elections in an easy-to-use Excel spreadsheet. This information can be submitted electronically via a secure website, and Colonial Life reconciles the bill to eliminate any additional work for the employer.
Delta Dental: Yes. Delta Dental has several billing and payment formats
available depending on the client’s plans and preference and will work with the client to determine the best process. The group sponsor is responsible for collecting the monthly premiums (through payroll deduction or automatic clearinghouse and submitting premiums and eligibility data each month.
Guardian: Yes. Guardian offers a single bill (online or in the mail) for all
Guardian coverages a client has to ensure the payment process is easy to manage.
MetLife: Yes. MetLife can allow for a single voluntary benefit deduction
for numerous benefits or separate deductions for each benefit on one bill.
Unum: Yes.
9.
Does your system offer online searches for employee policy status, coverage effective dates and policy/coverage type?
Aflac: We offer the Aflac Wingspan online service for policyholders.
Policyholders can log on to aflac.com 24/7 to do the following:
•
Check claim status.
•
Update their personal profiles.
•
Request forms or copies of their policies.
•
Obtain contact information for Aflac agents.
•
File claims quickly using Aflac SmartClaim.
Ameritas: Yes
Cigna: Yes.
Colonial Life: Yes. Colonial Life’s Ez Administration system offers online
searches for employee policy status, coverage effective dates and policy/coverage type.
Delta Dental: Yes. Delta Dental’s online eligibility application allows
benefit administrators to view and maintain coverage effective dates and coverage types, make real-time updates to eligibility data and improve the efficiency, accuracy and security of eligibility reporting. In addition, Delta Dental’s website, www.deltadentalins.com, provides a multitude of useful features to registered enrollees behind a secure sign-on, including the ability to view benefits and eligibility information, including coverage effective dates and coverage types; print ID cards; verify plan deductible and maximum information; and view claims status and claims history for the past 18 months
Health Net: Employees/members may confirm their coverage effective
date and policy/coverage type online or by calling Health Net’s Customer Contact Center.
Humana: The employee can go online to view any EOBs pertaining to
any of the health-based products.
Golden West Dental & Vision:N/A
Guardian: Yes, Guardian’s benefit website offers a one stop source for
plan administrators to manage their account online, including look ups for an employee’s policy status, coverage effective date and policy/coverage type.
MetLife: Our online billing system allows the employer to sort the bill by
different criteria.
Unum: No
10. Do you offer downloadable claim forms?
Aflac: Yes. Policyholders may download claim forms from aflac.com.
They also get tips on expediting forms and a direct link for sending a message to our Claims Department. Aflac also offers SmartClaim, an online claim filing process.
Ameritas: Yes
Cigna: Yes.
Colonial Life: Yes. Colonial Life provides claim forms on its web site at www.coloniallife.com that policyholders and plan administrators can download and print.
Delta Dental: Yes. Enrollees may download and print claim forms directly from our Website. However, Delta Dental dentists agree to submit claims on behalf of the enrollee and to accept payment directly from Delta Dental; therefore, the only time an enrollee may be responsible for submitting a claim form to Delta Dental is when treatment is provided by a non-Delta Dental dentist.
Golden West Dental & Vision: Yes.
Guardian: Yes, Guardian’s benefit website offers a one stop source for plan administrators to manage their account online, including the ability to download claim forms or e-mail a claim form directly to someone.
Health Net: Yes. Employees/members can find claims forms on
www.healthnet.com.
Humana: Yes. PDFs of all claim forms can be downloaded from the website.
MetLife: Yes. For several product offerings that require claim forms. MetLife Auto & Home even accepts towing claims online for many states.
Unum: Yes
11.
Do you require carrier reps. to have a comprehensive knowledge of all of the products they deal with?
Aflac: Yes. Training for Aflac agents hits every facet of Aflac’s plans and
sales cycle, such as field-tested scripts, brochures, one-on-one mentoring and online courses. Here are a few of the resources available to our agents:
•
New Associate Sales School (features comprehensive training sessions for new sales agents).
•
Ongoing training on new plans, services, and technology led by experienced trainers in a classroom setting.
•
Coaching and mentoring from sales managers and veteran agents.
•
Specialized training.
•
Continuing education via Aflac University courses online (provides product, leadership, and industry training for agents at their convenience).
•
Webinars and other online training materials available through Aflac’s Web site With the years of experience of Aflac’s District, Regional, and State Sales Coordinator and our extensive training, agents have the knowledge to provide the best service to your client and their employees.
Ameritas: Yes. Our reps are subject matter experts on all products
they sell.
Cigna: Yes.
Colonial Life: Yes. Colonial Life has a 10,000-member organization
of benefit professionals that covers the nation. They receive thorough product training through Colonial Life College on both voluntary products and the employer’s core benefits, at the employer’s discretion. A major part of our mission is to help employees understand their benefit program, help them uncover their insurance needs and help them select the coverage they need to protect their financial risk.
Delta Dental: Yes. Throughout the year, we provide support through
continuing education for consultants and brokers, such as lunch and learn presentations, CE courses and personalized support from our sales staff.
Golden West Dental & Vision: Yes.
Guardian: Yes. Guardian sales representatives achieve a high level
of comprehensive knowledge of the Guardian products they present through intensive and ongoing training. According to an independent survey conducted by JHA, producers rated us as exceeding the industry standard in the measurement of sales rep knowledge or product.
Health Net: Yes. Health Net’s Sales and Account Management teams
must have a comprehensive knowledge of all Health Net products that they offer and support.
Humana: Yes. Each sales representative must go through an extensive
sales learning academy, pass multiple tests, and continue to be accredited each year.
MetLife: Yes. Our licensed reps. specialize in voluntary benefits and
many have extensive experience in designing benefit programs.
Unum: Yes. We have an extensive training process, and sales reps
are expected have an extensive and comprehensive knowledge of our group and VB products. They’re first year is dedicated to development, with a 9-month self-directed process of activities and testing.
12.
How does your company support a good working relationships between brokers and carrier reps?
Aflac: Aflac offers complete insurance broker training, personalized support, sales materials, industry leading tools, and competitive compensation. Aflac is not about “once and done.” We are committed to providing continuous training, to our brokers, on the latest news and information, and presentations on industry topics and continuing education. In addition, our internal insurance broker team is always available to answer questions and provide personalized support.
Ameritas: Relationships are key with our brokers/producers. Our service is not just at the beginning of a sale; it remains throughout the process and for the life of the case. This takes great relationship skills among all partners.
Cigna: Simple: We help our brokers offer solutions to their clients. First, we offer products and services that meet a critical market need. Then, we support those products with pricing, service and materials that clearly communicate the value of what we offer. In addition, our sales force maintains regular contact with brokers through lunch and learn events and market events. We often partner with our parent organization, CIGNA Healthcare, to produce broker forums and other conferences.
Colonial Life: Working with and supporting brokers is a priority at Colonial Life. Our team of benefit professionals works with insurance brokers to help solve their clients’ benefit challenges. Colonial Life, recently appointed, regional broker marketing managers are dedicated to strengthening broker relationships nationally and regionally, supporting national alliance partners and interacting with worksite specialist brokers. Because of our dedication to broker marketing, brokers have named Colonial Life their top choice five years in a row in a nationwide readers’ survey conducted by Benefits Selling magazine.
Delta Dental: Delta Dental focuses on providing brokers and consultants easy access to their client’s data during the RFP and renewal process. We believe that we provide more hands-on service than any other dental carrier — both before and after the sale.
Golden West Dental & Vision: Our outside sales and service team is available for ongoing training and support with clients.
Guardian: With one of the longest-tenured sales forces in the employee
benefit industry, Guardian has a history of understanding the needs of growing businesses, which strengthens good working relationships. Guardian’s promise is to give brokers more ways to take good care of their clients. Our flexible and comprehensive product portfolio and responsive, personalized service support local relationships in delivering on this promise.
Health Net: To support the needs of our brokers and reps, Health Net has a dedicated account management team. We give small business group brokers direct access to account management teams responsible for specific territory and broker assignment/relationships. Brokers also have immediate, toll-free access to the Account Management team during business hours. In addition, our Account Service Unit within Health Net’s Customer Contact Center can provide claim and benefit information quickly.
Humana: Humana has a long history of strong relationships among brokers and our internal representatives. Brokers are integral to the success of our business and we provide opportunities, such as field advisory counsels, as a way for brokers to help develop the framework for developing new products and services that they believe are important to our employer groups. It is through these continued initiatives that we create a partnership between our sales associates, our brokers, employer groups and ultimately the employees.
MetLife: Our reps. work closely with brokers to help provide solutions that meet the needs of their clients.
Unum: Yes. Unum has strong relationships with its sales partners throughout the United States, with 40 field offices that provide local sales and service support. Unum provides broker training opportunities throughout the year, including CE course offerings. We publish a quarterly newsletter for brokers and welcome brokerage firms to the home offices for information sessions and tours of its claims and service operations.
13.
Do you offer marketing materials that are easy to present and simple for clients to understand?
Aflac: Your client’s Aflac service team is dedicated to working with them to ensure that the marketing campaign they select best suits their employees’ needs. All benefit education material is provided at no direct cost to your client. Here are a few ways we can educate your client’s employees about our plans and services: posters, flyers, brochures, payroll stuffers, flash presentations, an account specific website, employer Website information, newsletter articles, and e-mails.
Ameritas: Yes. Ameritas Group re-branded all our marketing material with the major objective to be easy to understand. This is maintained throughout all our material, including correspondence.
Colonial Life: Yes. Colonial Life realizes benefits and insurance terms can be complicated. Our marketing materials are easy to understand so employers can make better decisions on changes to their benefit programs and so employees can better understand their insurance needs and make better choices to meet those needs.
Cigna: Yes. CIGNA Voluntary is committed to improved communications with its customers through education and simplicity. Feedback gathered in focus groups and surveys has resulted in improved communication tools that help customers understand how limited-benefit medical plans work, the services available and how to maximize their health care dollars.
Delta Dental: Yes. We have a strong commitment to educating all of our customers. For brokers, consultants and benefit administrators, Delta Dental publishes an e-mail news-blast for key groups and brokers or consultants, a quarterly e-mail newsletter that provides dental benefit market news for brokers, consultants and general agents, and quarterly e-mail newsletter provides benefit administrators with the most up-to-date dental benefit news. Delta Dental also online features broker tools with information regarding: Our products, dental benefit pricing and sales, an RFP submission checklist, and a benefit administrator support guide.
Golden West Dental & Vision: Yes.
Guardian: Yes. From marketing materials shared with brokers to bound enrollment kits personalized to each employee and beyond, the foundation of Guardian’s communications are centered on being easy to present and simple for clients to understand.
Health Net: Yes. Health Net takes great pride in the ease of use of our marketing materials. For example, Health Net has received tremendous positive feedback from brokers on “the plan wheel,” a visual aid that helps small business group brokers better understand our full portfolio of plans.
Humana: Yes. We have a comprehensive suite of materials that brokers can present to employers and another set of materials that are designed specifically for the employees. Our research has shown that employees want benefits that are concise and easy to understand and our marketing materials reflect their needs.
MetLife: Yes. We offer a broad range of materials that are easy to understand and demonstrate the value of voluntary benefits to employees. MetLife will work closely with brokers and their clients to understand an employer’s workplace culture, communications style and preferences. This approach, coupled with our experience and knowledge of proven communications practices, will help to ensure that the simplest and most effective communications are implemented.
Unum: Yes
14.
How do you track the quality of the customer service you provide to employers? For example, you do set annual service goals and measure and report results?
Aflac: We constantly measure our customer satisfaction level with policy-
holders and business accounts in a variety of ways, such as surveys and audits. We monitor satisfaction with the total Aflac experience as well as satisfaction with enrollment, claims and billing. Our customer service quality program is administered by the Administrative Best Practices Quality Department. Each major business function, (i.e. primary, claims, and specialty) is sampled monthly. Additionally, for quality scoring, Administrative Best Practices guarantees a minimum of five audits per month for each customer service center representative. All scoring and error trending are reported weekly, monthly, and quarterly to management. Our Internal Audit Department also conducts audits by line of business in addition to their annual assessment of internal claims controls.
Ameritas: All Ameritas Group’s customer service is measured through
metrics down to the individual customer service associate. The tracking is done through our own systems and is based on all the major drivers of satisfaction for our customers. All metrics are integrated into our associates’ salaries to assure common drivers of service.
Cigna: Customer satisfaction is an extremely important component of
assessing the overall quality of service provided by CIGNA Voluntary. CIGNA Voluntary uses established annual service goals to evaluate the performance of our Customer Service Representatives. Through a partnership with Convergys, CIGNA Voluntary implements regular customer satisfaction surveys.
Colonial Life: Colonial Life provides superior customer service to all of our customer groups: brokers, employers and policyholders. We set internal annual customer service goals, measure our results quarterly and report the results on our web site. We also work with LIMRA to conduct quarterly or semiannual surveys of our plan administrators and policyholders and report those results. In addition, all employees who meet with a Colonial Life benefit counselor are asked to rate their one-to-one benefit counseling experience during their enrollment. Every account participating in the post-enrollment survey receives a report card with the survey results.
Delta Dental: To ensure we consistently provide quality customer service, Delta Dental records all incoming customer service calls verbatim and actively monitors a random sample of calls to identify areas for ongoing training and service improvement. Customer Service management is responsible for evaluating politeness, professionalism, responsiveness and accuracy of information provided. Service goals are tracked daily, measured globally and reported annually. Delta Dental also conducts random surveys of participants to measure their general satisfaction with Delta Dental and their benefit plans and costs, the professionalism of dentists and dental office staff and the treatment provided, customer service and claims processing
Guardian: Guardian sets service goals, and tracks and reports the results each year.
Health Net: Yes, Health Net sets goals and tracks performance against key service metrics. We also conduct customer satisfaction surveys about Health Net’s services and support. Information is also gathered on customers’ perceptions of other health care insurers to provide Health Net with competitive benchmarks.
Humana: Humana has established metrics for each division of the company. For example, our service goal for customer service is 98% and in 2008 our actual number was 99.7%. Our average claim time for disability claims is five days or less. We constantly audit all calls and look for ways to improve our metrics to exceed our customers’ expectations.
MetLife: We provide utilization and participation reports to employers at their request. We also monitor our customer satisfaction levels through our call center on an ongoing basis.
Unum: We certainly set goals around responsiveness and accuracy of service. We also have a quality assurance program that checks to see if we delivered our services in a timely and accurate manner as well. Additionally, we survey customers several times each year to better understand how they view their Unum experience.
15.
Do you have an established local sales and service team that can provide critical service in the same cities that the broker’s clients are in?
Aflac: Yes. Aflac is represented by more than 75,300 licensed independent sales agents and brokers throughout the United States, with more than 11,100 producing weekly (Aflac Annual Report for 2009). Our certified enrollers are available to service multi-location accounts and we have a national sales coordinator team to manage these relationships.
Ameritas: Yes, Ameritas has both local and remote service teams to provide all critical service. If claims information is needed after hours, our customer connections department is open until midnight central standard time.
Cigna: Yes, CIGNA Voluntary has established territories that are serviced by new business managers and client managers across the nation.
Colonial Life: Yes. Colonial Life has a national team of 10,000 benefit professionals who provide local enrollment support and service for our broker partners’ clients. For example, we have an account with 7,000 employees in 150 locations across the country. Our benefit counselors met locally with employees at each location and conducted individual counseling sessions. Because those benefit counselors live nearby, they can be on hand to help out with next year’s enrollment and any ongoing service needs. The goal is for our benefit counselors to build strong relationships with employees in the account.
Delta Dental: Every client is assigned a designated account manager who is responsible for overseeing program implementation, subsequent renewal activities, day-to-day issue resolution, and for participating in information meetings with benefit managers and enrollees as needed. Delta Dental of California has sales offices in San Francisco, Sacramento, Cerritos, San Diego and Fresno.
Golden West Dental & Vision: Yes.
Guardian: Guardian has over 55 local sales offices nationwide to support the needs of brokers and their clients.
Health Net: Yes, Health Net has several regional sales and service teams throughout California to support brokers and their clients.
Humana: We have account managers in most of our sales office (approximately 50 offices around the country) who can handle most calls as part of our single point of service. The claims and customer service team is primary in our Lancaster, South Carolina office, where 450 people are dedicated to our workplace voluntary benefits.
MetLife: Yes. We have representatives that specialize in voluntary benefits located in major cities throughout the U.S.
Unum: Yes. Unum has 40 local sales and service offices located throughout the U.S. with four locations in Calif.
16.
Do you have both a sales rep. and a service rep? (The sales rep helps the broker market and position products, manage blocks of business, and develop target markets and the service rep. helps implement and fulfill account enrollments.)
Aflac: In addition to a national sales coordinator team dedicated to
managing relationships, a local Aflac agent and their team will be available for services such as sales, and can also provide administrative and claims assistance. Additionally, we have a Market vice president who works directly with our broker development coordinators. For accounts with 500 or more employees, an account relations executive is assigned once the contract is signed. The account-relations executive will oversee a variety of services such as the following:
•
Acquisition and consultation
•
Welcome communications
•
Enrollment facilitation
•
Account visits
•
Account audits
Ameritas: Yes
Cigna: Yes. CIGNA Voluntary New Business Managers partner with
Brokers to present our product to prospective clients. Once a client chooses to offer CIGNA Voluntary products to their employees, we assign a dedicated client manager as well as a service team to implement the plans and provide ongoing service for day-to-day issues.
Colonial Life: Yes. Colonial Life’s national team of benefit professionals
have specialized roles they fulfill during the enrollment process. Benefits professionals work with brokers and their clients to help develop voluntary benefit strategies that will help clients’ solve their benefit challenges. Account coordinators help manage the enrollment logistics and report. And benefit counselors meet individually with each employee to educate them on their benefits, help them uncover any needs and select insurance plans to meet those needs.
Delta Dental: Yes. To ensure that our clients receive a high level of ser-
vice, Delta Dental uses a team approach to provide service and rapid response. A client’s team will include a sales account executive and an account manager. Together they are supported by account management specialists and administrative assistants.
Golden West Dental & Vision: Yes.
Guardian: Yes. Guardian has over 250 local sales representatives to help brokers market, over 120 benefit advisors dedicated to supporting enrollment efforts and customer services representatives available to serve the distinct needs of brokers and their clients.
Health Net: Yes. Health Net has both sales and service representatives to assist brokers and their clients.
Humana: Humana provides a dedicated team of account managers,
renewal specialists, and account installation managers to each case. We realize that much of the work begins after the case is sold and our goal is to provide dedicated resources for our clients for the duration of the case.
MetLife: Yes, we have a sales team and service team that work closely together to meet the needs of our brokers and customers.
Unum: Yes. Unum has more than 500 sales professionals across the
country, backed by a local service force of 1,000 professionals. The service team includes those who support Unum Enroll, our in-house enrollment team that supports voluntary benefit enrollment for employer groups of fewer than 500 lives.
17. Do you specialize in voluntary benefits?
Aflac: Yes. Aflac is a leader in guaranteed-renewable insurance policies
sold on a voluntary basis that pay cash benefits directly to policyholders, unless assigned. Currently, more than 443,000 employers make Aflac available to their employees. With a broad range of policies and value-added services, Aflac’s offerings suit virtually every business size and type. From three employees to 30,000, Aflac fits easily within any benefit package. Many times in the voluntary insurance business, companies tend to use the same approach to market similar benefits. Aflac is different. We back our unique plans up with the following:
•
Innovative marketing campaigns.
•
Strong financial stability.
•
Brand recognition.
•
A Solid company reputation.
•
Industry recognized and rewarded claims and customer service.
Ameritas: Yes. Ameritas has been providing voluntary benefits since
1990. We consider ourselves specialists in that arena because of our extremely high satisfaction levels from our customers and our constant systems evolutions to accommodate the needs of our customers. To specialize in voluntary benefits, we believe this is critical to achieve a win/win for all.
Cigna: Yes. CIGNA Voluntary’s mission is to improve the health and well
being of the working uninsured by providing affordable and easy-to-understand coverage. CIGNA Voluntary is the dedicated voluntary plan unit of CIGNA. We offer a premier package of voluntary plans across the country.
Colonial Life: Yes. Colonial Life, founded in 1939, began by selling ac-
cidental death coverage to individuals. In fact, the company pioneered the concept of offering voluntary benefits at the worksite in the 1950s. Colonial Life has always marketed only voluntary benefits, and during the 70 years it has been in business, the company has developed strong expertise and experience in the voluntary benefit industry.
Delta Dental: Delta Dental specializes in non-voluntary, partially volun-
tary and totally voluntary dental benefit programs.
Golden West Dental & Vision: Yes.
Guardian: Voluntary benefits are an incredibly important part of our group business. We do also offer plans that can be fully or partially funded by the employer.
Health Net: Health Net does not specialize in voluntary benefits. However, Health Net does offer the types of voluntary plans that are most commonly requested by our health plan customers.
Humana: Yes. Humana acquired Kanawha Insurance Company in 2007. Kanawha has been providing voluntary benefits for 50 years and is a licensed insurer in 48 jurisdictions.
MetLife: Yes. We and our affiliates have been offering voluntary benefits for over 30 years and have a broad suite of market-leading products.
Unum: Yes. Unum is ranked second in inforce premium in the voluntary benefit market as reported by Eastbridge Consulting Group in 2008. Unum leads the voluntary market in sales of critical illness insurance as well as universal and whole life insurance.
Health Reform Prompts Employers To Get Creative With Wellness
by Dr. Ann D. Clark
The epic debate on healthcare raised plenty of controversy and confusion, but one thing that people across both aisles seemed to agree on was the need for a renewed focus on wellness and prevention at the workplace, in schools and at home.
While wellness didn’t get nearly as much media coverage as other aspects of health reform provisions include grants for small businesses to implement wellness programs. It also requires qualified health plans to cover the cost of certain preventive care services and allows employers to increase incentives for participation in wellness programs to 30% of the cost of coverage, up from 20%.
These latest incentives in health reform are just one part of widespread wellness movement. The First Lady is championing the fight against childhood obesity with “Let’s Move;” millions of people tune in to watch “The Biggest Loser” each week; and celebrity chef Jamie Oliver takes on school cafeteria options in the popular TV show, “Jamie Oliver’s Food Revolution.”
This national momentum behind wellness is prompting more and more employers to start or expand wellness programs. In fact, a recent survey of 282 employers by Watson Wyatt and the National Business Group on health found that 72% were enhancing onsite programs aimed at stress management, EAPs or health coaching or plan to do so in the next 12 months. As workplace wellness programs become the increasing norm, the question is no longer “Why wellness?” but “How?” How does wellness work on a limited budget? How does a wellness program achieve maximum results? The answer begins with engagement. If employees don’t believe that it is in their best interest to prevent illness and make healthy lifestyle choices, they will have no interest in participating in wellness at the workplace. Achieving employee buy-in can be a major obstacle in wellness, as a recent Towers Watson survey found that 58% of employees lack engagement. To maximize employee engagement, wellness leaders need to involve employees in the entire wellness process, from preliminary planning through implementation.
Before launching a full-scale wellness initiative, the first question to ask employers is, “How well do you know your workforce?” Too often, brokers, HR and wellness leaders think they know exactly what employees need in a wellness program, but they never ask the employees themselves. A simple electronic survey will gather this imperative data and get employees engaged from the start. These surveys are extremely cost-effective, completely confidential, and employees appreciate the opportunity to provide input. This critical step in the planning process gives employers vital information and insight about what employees’ biggest health concerns are, what motivates employees, what communication and outreach will be most effective, and what employees think the wellness program should include.
Wellness Needs To Be Less Corporate, More Personal
The next step to maximizing employee engagement involves creating the message, and in essence, selling wellness to the workforce. With trust waning toward government, big business, and corporations, wellness cannot come across as a Big Brother program, created to financially benefit the corporation and access employees’ private information. The focus has to be less corporate, more personal. Companies have to offer wellness to employees because it is the right thing to do as an investment in employee well being, and a way to give back to employees for all their hard work and dedication. Wellness is supposed to help employees take control of their health. Employees don’t care about saving the company money; they only care how wellness benefits them. Employees would welcome a program designed to reduce stress, increase energy, strengthen personal resilience, and enhance quality of life. This message of individual empowerment and betterment needs to be clear and strong in all written, online, and verbal communication about the program. By crafting a strong marketing and communication strategy behind a wellness program launch, an organization prevents employee cynicism and skepticism and builds employee enthusiasm and excitement from the start.
An easy way to make the wellness message personal is to get employees involved in creating it. Companies can hold a contest to have employees come up with the best name or slogan for the wellness program and employees can all vote on the submissions. Another idea is to invite employees to share what motivates them to get well, “I want to fit into my pre-pregnancy skinny jeans,” “I want to walk my daughter down the aisle without getting out of breath,” “I want to blow people away at my 20-year reunion” or “I want to feel less exhausted at the end of the day.” Share these motivational statements with employees by posting them on the wellness website, flyers, t-shirts, or other wellness promotional materials. Have employees vote on the funniest, most inspiring, or most likely to succeed. Incorporating personal goals into the wellness message helps employees identify with the program and feel more inclined to engage in ongoing activities.
Get Creative With Communication and Outreach
In addition to a strong message and marketing campaign, it is important to ensure that the method of wellness communication is effective and reaches the maximum amount of employees. If employees have large populations of Hispanic employees, wellness materials should be provided in Spanish and Spanish-speaking staff should be available to administer BMI testing and answer questions at health fairs.
Some companies with large populations of off-site or remote employees need creative communication strategies to engage these employees.
Build Enthusiasm With Health Fairs and Annual Challenges
Creativity does not end with marketing and communication; the wellness program must get creative in the program launch, health fairs, and ongoing promotions and challenges to maintain enthusiasm and engagement. Health fairs and benefit orientations should be lively, with plenty of interactive elements like dance and yoga classes, massage chairs, great giveaways and other out-of-the-box elements. After an exciting launch, there should be an immediate and strong wellness promotion, like a Biggest Loser contest.
Challenges should be based on employees’ health goals in order to maximize engagement. It helps to involve employees in the development phase by creating workforce wellness committees focused on specific goals, such as the stress management team, the smoking cessation committee, and the healthy eating task force, for example. Employees, of all levels, can work together to develop the best strategies to tackle these major wellness goals, share best practices, and brainstorm on creative challenges, promotions and incentives that would work best. Employees involved in the wellness planning and implementation help generate buzz throughout the workforce, and are more invested in wellness success.
Shift the Discussion to Ensure Leadership Buy-In
When it comes to executives, the wellness discussion often gets stuck in a numbers game. What is the projected return-on-investment in year one, year two, year five? What is the financial impact on healthcare costs? While these are all important business questions, there exists countless data, research and case studies that consistently confirm the financial benefit of wellness programs. It’s time for a major shift in the conversation. It’s time to ask leadership their thoughts on wellness, stress management, family health, preventive care, and health education; and what role the company has in fostering a healthy work environment.
A good indicator of a workplace that is ready for wellness is one that already has other healthy initiatives in place like an employee assistance program, work/life programs, concierge services, and safety training. If leadership believes that these programs help attract and retain employees while building a healthy and more productive workforce, they will be more inclined to buy into workplace wellness. Leadership buy-in requires more than lip service though, it requires action. Considering that executives generally set the tone for everything from work styles to dress codes, when they serve as an example of wellness, employees will follow.
Leadership also likes instant gratification, which can be a bit of a challenge in the beginning of the wellness process. When reporting wellness outcomes, it is important to keep the focus on engagement success and include employee feedback, survey results, success stories, participation rates and other engagement-related information and results. Another often overlooked component to wellness reporting is the number of employees “who didn’t get worse,” or in other words, employees who maintained good health, which is an extremely important factor in prevention and wellness success. The bottom line is that wellness success begins and ends with employee engagement. When employees are excited about wellness, they take the message home to families, support co-workers in healthy initiatives, and become part of the solution.
––––––––––
Dr. Ann D. Clark is CEO and Founder of ACI Specialty Benefits, a Top 10 EAP and leading provider of student assistance programs, wellness, concierge and work/life services. A best-selling author, Dr. Clark is one of the original Certified Employee Assistance Professionals (CEAP) and a licensed Marriage and Family Therapist. She can be contacted at aclark@acispecialtybenefits.com.
The Use of Virtual Counseling to Communicate Life Insurance Options
by Harry Gottlieb
As a life insurance professional, think about when you last selected a life insurance plan for yourself and how you went about doing it. You took into consideration your family size, the annual income of your spouse, and whether your kids were bound for Princeton or your nearest in-state college. You crunched some numbers to figure inflation, taxes – all the important stuff. You knew what you were doing and you knew what questions to ask yourself.
So now let’s take a look at where people who aren’t life insurance professionals turn to for life insurance advice. Ideally, they come to you, right? Well, here’s the problem. The Life Insurance and Market Research Association (LIMRA) reports that 63% of all Americans with some sort of coverage either received it or purchased it through their jobs. This means that chances are very good these people have not spoken directly with an insurance broker about their decisions. They read whatever information their employer gives them and maybe do some independent research. Very few actually consult with a financial planner. Wouldn’t it be amazing if you could be that financial advisor? No matter where or when a person has a life insurance question, you could swoop in and answer it for them. Sure, you’d have to bend space-time to do it, but you could certainly help a lot of people.
Fortunately, there is a new trend in benefits education called “Personalized Guidance.” It’s a computer interface that allows brokers to offer their clients online, personalized insurance guidance for employees. The virtual counselor knows the right questions to ask about family size, financial details, and personal priorities. If it is designed well, it knows how to make sure that the employee is learning enough to make educated life insurance decisions.
Creating an engaging virtual counselor requires far more than simply putting a fill-in-the-blank form up on a website and directing employees to fill it out. There are lots of online calculators for life insurance and some even explain some of the more opaque terminology, such as “final expenses.” But very few know how to literally speak to the person in front of the screen. Virtual counselors are created by stringing media files together to create a dynamic and memorable experience — one that feels like the online counselor is speaking directly to the employee. When done well, the virtual counselor talks in a relatable and realistic tone and manner, speaking in non-technical English so that a person with little to no knowledge of life insurance can easily understand. For example, “final expenses” is explained as funeral expenses that yes, no one likes to think about, “but don’t you want that awful, final bill to be one less thing your family needs to worry about?” Then the virtual counselor can calculate the estimated funeral expenses into the employee’s needed life insurance coverage.
There are plenty of advantages to providing virtual counseling over other forms of employee education. Here are some of my favorites:
1.
Virtual counseling sets you apart — Employers know that there is a need for education about employee benefits and that it is in their best interest to go with a broker that can help them provide this education. A recent MetLife study revealed that 58% of employees polled wanted their employer to provide access to financial planning tools, including tool to determine what benefits they really need.
Offering virtual counseling tools makes you stand out from all the others. Most HR departments are strapped for time and money. If you save the day by providing a strong employee education and communication tool like virtual counseling, you will be offering them a valuable service – one that will be remembered long after their open enrollment is complete.
2. Better education leads to better enrollment in supplemental life insurance — By providing individualized education, employees can learn exactly how much life insurance coverage they need for their families. As you know, this amount is usually much higher than the basic coverage provided by the employer, especially for families with small children or families with one breadwinner. If an employee knows this, it can lead to higher enrollment in supplemental insurance. When the maximum for supplemental isn’t enough, the virtual counselor can direct them to where they can purchase additional life insurance from a broker – like let’s say….you.
3.
Virtual counseling puts people at ease — Life insurance can rattle a lot of people. These are big decisions that affect the people they love and care about more than anything in the world. And let’s be honest here: people don’t like to think about their own mortality. Virtual counseling allows people to learn about their life insurance needs and options in their own homes, on their own time, with a spouse or partner present to discuss options. Employees need life insurance education and employers need brokers to help do the educating. Virtual counseling provides an interactive conversation that is accessible to each and every employee. By providing this tool to your clients, you extend yourself directly to the individual employees themselves. For your clients who are hearing the appreciation from their employees, you will have their gratitude and loyalty. And who doesn’t want that?
––––––––––
Harry Gottlieb is the founder and CEO of The Jellyvision Lab, the Interactive Conversation Company known for creating the hit game, You Don’t Know Jack. The company creates interactive, rich media experiences to communicate complex subjects. For more information or to view a demo of the Jellyvision Benefits Counselor, please visit: http://www.jellyvisionbenefitscounselor.com.
Why Your Clients Need Medical Evacuation Benefits
by Brendan Sharkey
As your clients travel the world, are they properly protected against financial exposure due to catastrophic medical events? If they don’t secure comprehensive international medical benefits and assistance services before they go, they may find themselves exposed to huge losses — both physical and financial.
Though illness or injury can strike at any time, when severe incidents occur overseas, lack of proper coverage can leave travelers with steep medical bills for less than sufficient care. Proper coverage is international health insurance. These policies pay for doctor and hospital care for short or long trips and will supplement your client’s domestic plan. International health insurance can also be purchased as primary insurance for someone relocating to another country for an extended period and can include added features, such as preventative services, acupuncture, chiropractic, and maternity benefits. In addition, global travelers need to be prepared for the possibility that they may find themselves in a location where the medical care is poor or inaccessible and it is necessary to be evacuated to an area where they can receive the necessary level of care. Medical evacuations can be complicated and costly. However, most travel insurance plans include a medical assistance benefit, which is critical. It gives members 24/7/365 access to a company that will arrange the evacuation and coordinate appropriate treatment along the way.
Many domestic health insurance plans offer inadequate services and protection when taken abroad, this can be devastating when medical evacuation is necessary, which is almost never covered. Help your clients understand that the most comprehensive and reliable coverage comes in the form of an A-rated travel health insurance policy approved by state insurance regulators, so-called “admitted” plans. In contrast to benefits provided by medical evacuation membership programs, these policies include the benefits and services that give travelers the level of protection and assistance they need to travel with peace of mind.
Admitted plans have been approved by the state insurance department and are bound by state financial solvency requirements. Consumers who purchase admitted plans are less likely to encounter unexpected waiting periods, harsh exclusions, penalties, or unusual claims payment procedures. Admitted travel health insurance policies must meet minimum benefit requirements, which gives consumers the coverage they need. It also ensures that legitimate claims will be paid. Medical evacuation membership plans are not admitted insurance products and are not held to the same high standard for financial stability or consumer protection. Buying a more comprehensive travel health plan also promotes more appropriate medical care. The key considerations of any medical evacuation process involve more than a promise to evacuate members to the hospital of their choice. Evacuating a patient for medical reasons is a complex process that includes that following:
•
Evaluating the appropriateness of local healthcare providers.
•
Identifying the closest facility where a high level of care is available.
•
Determining the risk and rewards of moving the patient.
•
Choosing the best method of transport (for example, ambulance, helicopter, fixed wing air ambulance).
•
Securing the cooperation of the local treating physician, including a determination that the patient is stable enough to be moved.
•
Enlisting the most appropriate team to handle the transport (for example, doctor, nurse, therapist)..
•
Arranging for speedy and appropriate intake at the receiving facility.
Unless the medical assistance staff and the travel health insurance benefits address all of these points, the medical evacuation event could go off track or languish while arrangements are made to stabilize the patient and pay for medical treatment upfront.
Membership plans that promise evacuation to “your hospital of choice” often require inpatients to be discharged, transported, and readmitted. This means that a patient would be admitted for treatment in an initial location, then discharged for the medical transport, and then taken to a facility and admitted for necessary further treatment. This scenario accounts for less than 1% of the medical assistance cases that arise overseas. For instance, if the patient has an appendectomy, once the appendix is removed, readmission to another facility would not likely be required and so an evacuation would likely not be covered.
Comprehensive benefits also allow for easier admittance and discharge when dealing with international hospitals. Getting healthcare can be tricky in some parts of the world. Some hospitals won’t provide any treatment or won’t allow a patient to be discharged until the hospital has received a guarantee of payment for the services they provide. Such guarantees are commonly provided by travel insurers along with assistance providers, but rarely by other insurers or managed care plans. Without the coverage provided by a company that can secure the guarantee, a traveler who needs immediate care will have to pay the facility, in advance, perhaps as much as tens of thousands of dollars. And for those who have to pay with a credit card, there is a chance that the hospital won’t accept foreign credit cards or that the credit card won’t have a sufficient credit limit. Admitted travel health insurance plans provide evacuation and other comprehensive benefits and assistance that address the following issues:
•
In a true medical emergency, your clients won’t be fit to fly. They will need to get excellent local hospital care first and an assistance staff that can work with the hospital to arrange the necessary guarantee of payment for treatment.
•
Coverage for necessary physician services, prescription drugs and ancillary medical care.
•
Referrals and access to the most skilled and appropriate doctors.
•
Protection that the consumer will have the proper level of benefits and that claims resulting from this coverage will be paid in a timely manner.
Don’t sell your clients short. Make sure you offer them a full service, admitted travel health plan that provides a higher level of protection and peace of mind than evacuation membership plans do.
––––––––––
Brendan Sharkey is director of individual travel programs for HTH Worldwide in Radnor, Penn. His most recent contributions include CNBC Morning Television, The Wall Street Journal, USA Today, Consumer Reports Magazine, the Los Angeles Times and the Washington Post, among others. Brendan has partnerships in the online travel, benefit platform and search engine arena including Yahoo and Frommer’s. Brendan has lived in Scotland, Canada, and Australia and holds a Bachelor of Commerce (Marketing) from Griffith University in Australia. Contact him at bsharkey@hthworldwide.com.
Conference Highlights the Growth of Medical Tourism
by Leila Morris
The recent Medical Tourism & Global Healthcare Congress in Los Angeles attracted more than 1,200 from over 84 countries. The third annual conference was organized by the Medical Tourism Association. Jerry Turney, president of The Consolidated Marketing Group, LLC explained the reasons why medical tourism has become an accepted alternative to U.S. care.
Fifty four percent of Hispanics and 57% of Asians in the United States would consider going overseas for medical care, according to the Medical Tourism Assn. Turney noted the following advantages for self- insured employers and employees:
Employers
•
Claims cost savings of 50% to 80% on major procedures.
•
Lower stop-loss claims and premiums.
•
Increased benefits for employees and their dependents and reduced overall health plan costs.
•
Culturally desirable care for ethnic employees and their families.
•
An alternative to shifting costs to employees.
Employees
•
A money-saving alternative to US-based care with no compromise in quality.
•
Plan designs can include no deductibles, no coinsurance, no co-pays, and no out-of-pocket travel expenses
•
Employees choose freely between U.S. domestic treatment and the international medical benefits program. ·
•
Ethnic employees can get treatment in culturally familiar surroundings while enjoying reduced out-of-pocket costs.
Many international facilities are superior to U.S. facilities when measured by infection rates, survival rates, and other common factors, he explained. In addition, it is not unusual for medical treatments to be available internationally that have not been approved in the U.S. due to our cumbersome bureaucratic approval processes. One example is hip resurfacing, which is often superior to hip replacement. Since it’s been a routine procedure internationally for more than 10 years, surgeons in India and countries have a decade or more of experience over U.S. surgeons. Turney explained that many patients prefer to have care in culturally familiar surroundings and they view voluntary international care as a highly desirable employee benefit.
Then there are also the obvious economic draws to medical tourism. It is not unusual for charges in top-rated international facilities to be as little as 30% of U.S. treatment costs. “The typical private room rate in a Mexico City first tier hospital is only $250 per day,” he noted.
To encourage the use of international facilities, many employers adapt their plan document to waive deductibles and coinsurance for international care and will assist with transportation costs on major procedures exceeding a predetermined cost threshold.
Types of Available Programs
Medical tourism programs fall into several different categories, Turney explained. The embedded informational program provides general information on the international medical treatment option, but does not offer the personal concierge services of a medical travel facilitator. A Website presents information on international medical options. This option is popular with Trade and Ethnic Affinity Groups that provide it as a value-added program embedded into the association dues.
Turnkey programs include the services of a medical travel facilitator with an emphasis on ease of installation and cost effectiveness. Employee meetings and on-going communication are priorities. The medical travel facilitator can be reached by e-mail or phone. Plan documents are adapted to provide incentives as well as annual utilization. The facilitator coordinates with the health plan administrator. The facilitator provides help obtaining medical stop loss assistance, as needed.
A full customized program includes historical claims analysis, suggested revisions to plan documents to provide treatment incentives, ongoing reporting of plan performance, and coordination with the plan administrator. It includes full support services for initial program installation and ongoing management as well as coordination with the group’s medical stop loss carrier. Wouter Hoeberechts, CEO of World Med Assist said that, when looking at medical tourism for employees, plan sponsors should consider several issues to manage risk.
Members must be educated with explicit language that spells out their choices. Patients must be required to sign waivers before they travel. Fiduciary responsibility involves due diligence on selecting a medical travel facilitator. A medical travel insurance policy should do the following:
•
Provide protection against medical complications.
•
Cover of medical expenses.
•
Include other coverage (e.g. AD&D, lost luggage).
•
Be paid by the employer.
An employer liability policy should be for the entire plan, including the medical travel benefit it should offer professional liability and vicarious liability coverage. Hoeberechts said that overseas hospitals and provider networks should feature the following elements:
•
International accreditation.
•
In depth cooperation with major U.S. medical institutions.
•
Internationally renowned and trained doctors.
•
Surgical outcomes on par/above U.S. standards.
•
Use of latest medical technology (e.g. CyberKnife, da Vinci).
•
High staff/patient ratios; patient-centric orientation.
•
Experience in treating western patients.
•
English speaking staff; English language signage.
•
Good hotels close by or integrated into facility.
•
Geographical/cultural spread: portfolio approach.
•
All hospitals undergo rigorous credentialing process.
•
including on-site visits.
Judging from the growth of the conference in just three years, it won’t be long before employers and health plans work out many of these issues to make medical tourism a common and accepted option to deal with climbing health insurance costs.
––––––––––
Leila Morris is editor of California Broker Magazine.